Why Do We Sleep, and What Are the Dangers of Not Getting Enough?
I just finished reading the New York Times bestseller Why We Sleep by neuroscientist Matthew Walker, and it was fantastic. Sleep is essential for all aspects of health—from maintaining immune system, cardiovascular, and reproductive function to improving memory and preventing cancer, psychiatric disorders, and neurodegenerative decline. Yet the importance of sleep is vastly under-recognized, and we’re paying the price.
A National Sleep Foundation survey found that in the US, Canada, UK, Germany, and Japan, at least 50% of people don’t get sufficient sleep on weekdays. For most people, that means less than 7 hours. If you lead a busy life and routinely get 5 to 6 hours of sleep, you may feel pretty good about that. Unfortunately, studies consistently show the negative health effects of regularly sleeping 6 or fewer hours per night. And as Walker explains in his book, trying to catch up on sleep on the weekends doesn’t work; the damage has already been done.
If you think you’re one of those people who can function optimally on less sleep than the rest of us—you’re probably not. Less than 1% of people carry a gene, DEC2, which allows them to survive on less than five to six hours of sleep and experience minimal impairment in functioning. Walker writes that it is far more likely that you’ll be struck by lightning than have this gene.
Walker discusses every aspect of sleep you can think of in his outstanding book. His readable writing style and British wit made it hard for me to put down. In this post I’ll highlight some of the most important things I learned from the book. If you want to learn more, or if you need any further motivation to get a good night’s sleep, I highly recommend reading Why We Sleep.
REM vs. NREM sleep, and why we need both
Non-rapid eye movement sleep, referred to as NREM sleep, is characterized by our slowest brain waves. In contrast, during rapid eye movement (REM) sleep, brain activity is almost identical to when we’re awake. We cycle through REM sleep and four stages of NREM sleep approximately every 90 minutes throughout the night.
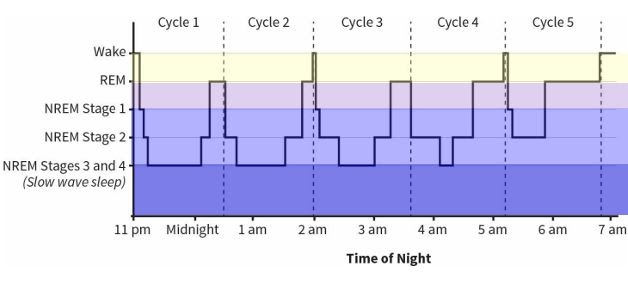
Figure 8: The Architecture of Sleep from Why We Sleep
Scientists agree that NREM sleep appeared first in evolution. Sleep studies on insects, amphibians, fish, and most reptiles don’t show concrete evidence of REM sleep. Birds and mammals, which evolved later, are the only species that exhibit true REM sleep.
REM sleep is when we dream. This is when our brain takes all of the information we’ve received during the day and processes it, integrating it with our past experiences. In doing so, REM sleep creates associative networks throughout our brain, building a framework for understanding our life and the world around us, and giving us insights and the ability to solve problems.
Dreaming is also essential for processing emotions and regulating emotional circuits. Studies by Dr. Rosalind Cartwright have shown how dreaming about traumatic events that we’ve experienced allows us to process and move past them, resulting in recovery from depression and anxiety. And research by Dr. Murray Raskind showed that reducing noradrenaline in the brain allowed PTSD patients to finally obtain REM sleep, which resulted in their flashbacks ceasing.
By contrast, in NREM sleep, we do not dream. NREM sleep is when our brains store and strengthen the memories of what we learned—this is known as memory consolidation. Not surprisingly, lack of memory consolidation is one of the two reasons that inadequate NREM sleep is associated with Alzheimer’s disease. The other reason is fascinating: Dr. Maiken Nedergaard discovered that during NREM sleep, glial cells (the brain’s support cells) shrink by up to 60%, and cerebrospinal fluid bathes the brain, clearing out metabolic debris. If this cleansing doesn’t occur, wastes including amyloid protein, tau protein, and other toxic metabolites build up in the brain, contributing to the development of Alzheimer’s disease.
NREM sleep also plays an essential role in the maturation of the brain during adolescence and into adulthood. Knowing this, we ought to make sleep a priority for our teenagers—but unfortunately, we’re often misinformed about how best to do this, and school schedules don’t help. During adolescence, circadian rhythms shift several hours later; so, teens don’t naturally get tired until around 11:00pm. They need more sleep than adults—on average, 9.25 hours—and their brains produce melatonin from 11:00pm to 8:00am. Unfortunately, most high schools start between 7:00 and 8:00am, when teens should still be in bed.
When Edina, Minnesota shifted their high school start time from 7:20am to 8:30am, it resulted in a dramatic increase in SAT scores. The average score among top-performing students went from 605 to 761 on the verbal portion of the test, and from 683 to 739 on the math portion. Attendance and graduation rates went up significantly, students reported less depression, school nurses reported better student health, and 92% of parents reported that their teens were easier to live with. Similar results have been reported in other counties and states where school start times have been shifted later.
(If you’re looking for guidance on sleep patterns for infants and children, I highly recommend Healthy Sleep Habits, Happy Child by Dr. Marc Weissbluth.)
How much and when should adults be sleeping for optimal health?
Walker explains that adults need an average of 8 hours of sleep per night to maintain optimal health. Other sources such as the National Sleep Foundation, The American Academy of Sleep Medicine, and the Sleep Research Society recommend between 7 and 9 hours or at least 7 hours per night.
I was very interested to learn that humans are biologically hardwired to sleep in a biphasic pattern, rather than the monophasic pattern that most of us adhere to. Monophasic sleep is when we attempt to get all our sleep in one long stretch. Biphasic sleep means that we have two periods of sleep in a 24-hour day. All humans experience a “genetically hardwired dip in alertness” in the mid-afternoon, called the “post-prandial alertness dip.” We function best when we take a short nap, 30 to 60 minutes long, during this afternoon period. We should then get the rest of our sleep overnight.
Some cultures in Mediterranean Europe and South America still allow for an afternoon siesta in their daily schedule. Sadly, when the afternoon nap is removed, there can be dire health consequences. Researchers from Harvard University’s School of Public Health followed more than 23,000 Greek adults over a six-year period, during which the practice of siesta was coming to an end for some of them. The researchers found that people who continued to take afternoon naps had a 37% lower risk of death from heart disease than those who did not take naps. Working men in particular benefited from an afternoon nap, showing a 60% reduced risk of death from heart disease.
Walker recommends taking your siesta in the early afternoon rather than in the late afternoon or evening. The nap clears away the “sleep pressure” created by the buildup of adenosine (which I’ll explain in the next section) so taking a nap later in the day makes it more difficult to fall asleep at night.
How caffeine and alcohol affect our sleep
Having been a coffee drinker for 23 years, and having recently quit, I was very interested to learn exactly why caffeine helps us feel alert and energized.
From the time we wake up and throughout the day, a chemical called adenosine continually builds up in our brains. Adenosine creates the desire to sleep. The longer we’re awake, the more adenosine builds up, and the more sleep pressure we feel.
Caffeine latches on to adenosine receptors in the brain, blocking the sleep signals that adenosine is trying to send to the brain. This is why caffeine makes us feel awake—for a period of time. But while we’re experiencing the wonderful high of caffeine, adenosine continues to build up. As our bodies metabolize the caffeine and its effects wear off, we experience a caffeine crash. The effects of all of the adenosine that has continued to build up is suddenly felt.
Overnight as we sleep, our brains degrade and remove the adenosine that has built up throughout the day. If we get approximately 8 hours of sleep, we’re able to completely clear the adenosine from our brains, allowing us to feel alert in the morning.
The half-life of caffeine, which is the length of time it takes our bodies to metabolize and clear away half of the dose of caffeine we’ve ingested, is approximately 5 hours. However, this length of time varies widely among individuals, ranging from 1.5 to 9.5 hours. This variance explains why some people can drink coffee right before bed and still fall asleep soundly, whereas others, like myself, are kept awake at night by a cup of coffee at lunchtime.
Consuming caffeine to the point that it affects your sleep at night is dangerous, because it’s all too easy to get into a cycle where you never get enough quality sleep to completely clear the adenosine from your brain. As I and many others have experienced, this quickly leads to caffeine dependency. If you’re an average person and your body clears 50% of caffeine from your system within 5 hours, keep in mind that half a dose of caffeine is enough to keep you up at night. Another 5 hours later, the quarter-dose of caffeine that remains in your system is enough to affect your sleep as well.
Now on to alcohol, which many people believe helps them sleep better. While alcohol is a sedative, slowing the firing of neurons in the brain, it does not induce natural sleep. Walker explains that its effect on brain activity is more like a light dose of anesthesia.
Sleep studies show that when we go to bed with alcohol in our system, the second half of our night of sleep is significantly disrupted. We briefly wake up many times, so our sleep is not continuous and not restorative. Most people don’t remember these awakenings, so they don’t realize that their evening drink is the cause of their grogginess the next morning. These disruptions during the second half of the night also result in a loss of important REM sleep.
Alcohol, even in moderate consumption, is a powerful suppressor of REM sleep. Walker describes a study of college students that clearly showed the negative effect of alcohol and the resulting loss of REM sleep on retention of academic material they had just learned. When students drank a moderate amount of alcohol on the first night after they had learned the new material, they only retained 50% of the information as compared to the control group, who did not drink. But more surprising was the result of a third group of students, who had two nights of natural, sober sleep after learning the new material. On the third night, they drank a moderate amount of alcohol. They then experienced a 40% loss of the new material they had learned 3 days before—almost as much as the students who had drank on the first night.
The health effects of chronic sleep deprivation
Chronic loss of sleep, which results from getting less than 6 to 7 hours of sleep on a regular basis, is associated with a wide range of conditions.
-
It weakens the immune system: People who sleep 6 hours or less per night are 4 times more likely to catch a cold than those who sleep at least 7 hours per night
-
It increases the risk of cancer: Walker describes a European study of almost 25,000 people which found that sleeping six hours or less per night was associated with a 40% increased risk of cancer, compared to people who slept 7 hours or more per night. Other studies have found a 50% increased risk of colorectal cancer, a 62% increased risk of breast cancer, and a 90% increased risk of prostate cancer among people who sleep 6 or fewer hours per night. And just one night of only 4 hours of sleep results in a loss of 72% of the natural killer cells of the immune system—our first line of defense against dangerous invaders such as cancer cells.
-
It leads to cognitive decline: People with insomnia are more than twice as likely to develop Alzheimer’s disease And in healthy adults, chronic sleep deprivation causes parts of the brain involved in learning and memory to shrink and their short-term memory to be impaired.
-
It affects fertility: Men who experience sleep disturbances have a 29% lower sperm count, and women who get less than 6 hours of sleep per night have 20% less follicular-releasing hormone, than those who get regular, full nights of sleep. And sleep-deprived men have significantly lower testosterone levels, equivalent to aging 10 to 15 years, while sleep-deprived women are more likely to have irregular menstrual cycles and experience infertility.
-
It increases the risk of cardiovascular disease: A 2011 study that tracked more than half a million people across 8 countries found that getting less sleep was associated with a 45% increased risk of developing or dying from coronary heart disease, independent of other lifestyle factors. A Japanese study of 4,000 men found an alarming 400-500% increased risk of heart attack among men who slept six hours or less as compared to men who slept more than six hours. Sleep loss makes the sympathetic nervous system overactive, resulting in an immediate increase in heart rate and blood pressure, weakened blood vessels, and a 200-300% increased risk of atherosclerosis (hardening of the arteries).
-
It increases the risk of diabetes: Research shows that after just 6 days of sleeping 4 hours per night, previously healthy volunteers develop pre-diabetic blood sugar levels; their cells become insulin-resistant after just one week of sleep loss.
-
It increases appetite and leads to weight gain: Sleep loss immediately leads to a decrease in leptin (the hormone that makes us feel full) and an increase in ghrelin (the hormone that makes us feel hungry), making sleep-deprived people consume more calories than those who get sufficient sleep. Sleep loss also increases levels of endocannabinoids in the body, giving us “the munchies” and making us more likely to snack.
-
It increases emotional reactivity and risk of psychiatric disorders and substance abuse: After just one night of sleep deprivation, the amygdala (a part of the brain central to stress and strong emotions) becomes more than 60% more reactive, and the prefrontal cortex (which helps to regulate the amygdala) becomes less active. After just three nights of restricted REM sleep, people become anxious, moody, paranoid, and have hallucinations. Sleep loss also makes the brain’s reward system hyperactive, leading people to pursue pleasure in the form of drugs and alcohol.
What should you do if you have insomnia?
Researchers have determined that insomnia—defined as having the opportunity to sleep but being unable to fall asleep and/or stay asleep—is most commonly caused by emotional concerns and psychological stress. If you have insomnia, this probably doesn’t come as a surprise. When you’re lying awake in bed at night with your mind racing, you know that you just need to let your mind slow down and relax so that you can fall asleep—but allowing that to happen can be challenging to impossible.
Brain scans of insomnia sufferers show that regions of the brain that generate emotions, recall memories, and maintain vigilance all remain active while trying to fall asleep, preventing the onset of sleep. And when they do fall asleep, insomnia sufferers have shallow NREM sleep and fragmented REM sleep, leading them to feel unrefreshed the next day.
Melatonin is an attractive option because it’s natural and free from the side effects of prescription sleep aids. Walker explains that melatonin helps to regulate the timing of when sleep occurs, but does not actually generate sleep. He believes that melatonin is most useful when dealing with jet lag and having to adjust to a new time zone. He also warns that over-the-counter melatonin pills can have much higher or lower concentrations of actual melatonin than advertised. But on the upside, Walker suggests that the placebo effect of melatonin is significant and should not be underestimated.
Walker does not recommend prescription sleeping pills, and he makes a clear case for why. Sleeping pills are sedatives, just as alcohol is, and they have the same effect: they slow neuronal firing and basically knock out higher regions of the brain. They do not induce natural sleep, and they also lead to grogginess the following day, forgetfulness, slowed reaction times, and performing actions at night that you do not remember the next day. The grogginess can lead people to become increasingly dependent on caffeine, making the sleeping pills more necessary. And when people stop taking sleeping pills, they often suffer from rebound insomnia as they withdraw from the addictive drugs. People who regularly take sleeping pills are 3.6 to 5.3 times more likely to die than those who don’t; the most common causes are infection, fatal car accidents, and cancer.
Non-pharmacological treatments for sleep are becoming more popular, and one in particular has proven to be more effective than drugs. Cognitive behavioral therapy for insomnia (CBT-I) has been shown in many clinical studies to be more effective than prescription sleep aids in helping people to fall asleep faster, sleep longer, and get better quality sleep. The effects of CBT-I are long-term and persist after treatment has ended. And best of all, there are no dangerous side effects.
The efficacy of CBT-I is so undeniable that in 2016, the American College of Physicians declared that CBT-I should be used as the first-line treatment for all individuals suffering from insomnia, not sleeping pills. You can learn more about CBT-I in this article on the Sleep Foundation website, and by searching for a CBT-I trained provider near you.
Want to learn more?
There are still more fascinating things to learn in Walker’s book: how our sleep cycles evolved, the dangers of driving while sleep-deprived, how two global catastrophes were caused by lack of sleep, how technology may improve our sleep, why Walker believes that sleep is more important for our health than diet and exercise, and his 12 Tips for Healthy Sleep.
If you want to learn more about why we sleep and the dangers of not getting enough sleep, or if you still need motivation to get a good night’s sleep, I highly recommend reading Why We Sleep!
Recommended reading:
The Pain Relief Secret: How to Retrain Your Nervous System, Heal Your Body, and Overcome Chronic Pain by Sarah Warren, CSE
Somatics: Reawakening the Mind’s Control of Movement, Flexibility and Health by Thomas Hanna

