What is the Polyvagal Theory?
The Polyvagal Theory is a theory proposed by Stephen Porges that describes how the mammalian autonomic nervous system evolved to keep us safe and alive. As mammals evolved from reptiles, our autonomic nervous system developed to automatically communicate with other mammals and engage different self-defense systems when needed.
When our self-defense systems are repeatedly or chronically engaged or we aren’t able to communicate with others effectively, our bodily systems can become stuck in certain maladaptive states. Porges’ theory emphasizes the importance of how our physiological state—the way the systems of our body are functioning—is involved in behavioral problems and psychiatric disorders.
In this post, I’ll explain the basics of the vagus nerve and Polyvagal Theory. In next month’s post, I’ll discuss how Polyvagal Theory can be used in clinical settings to help people overcome the lasting effects of trauma.
What is the vagus nerve?
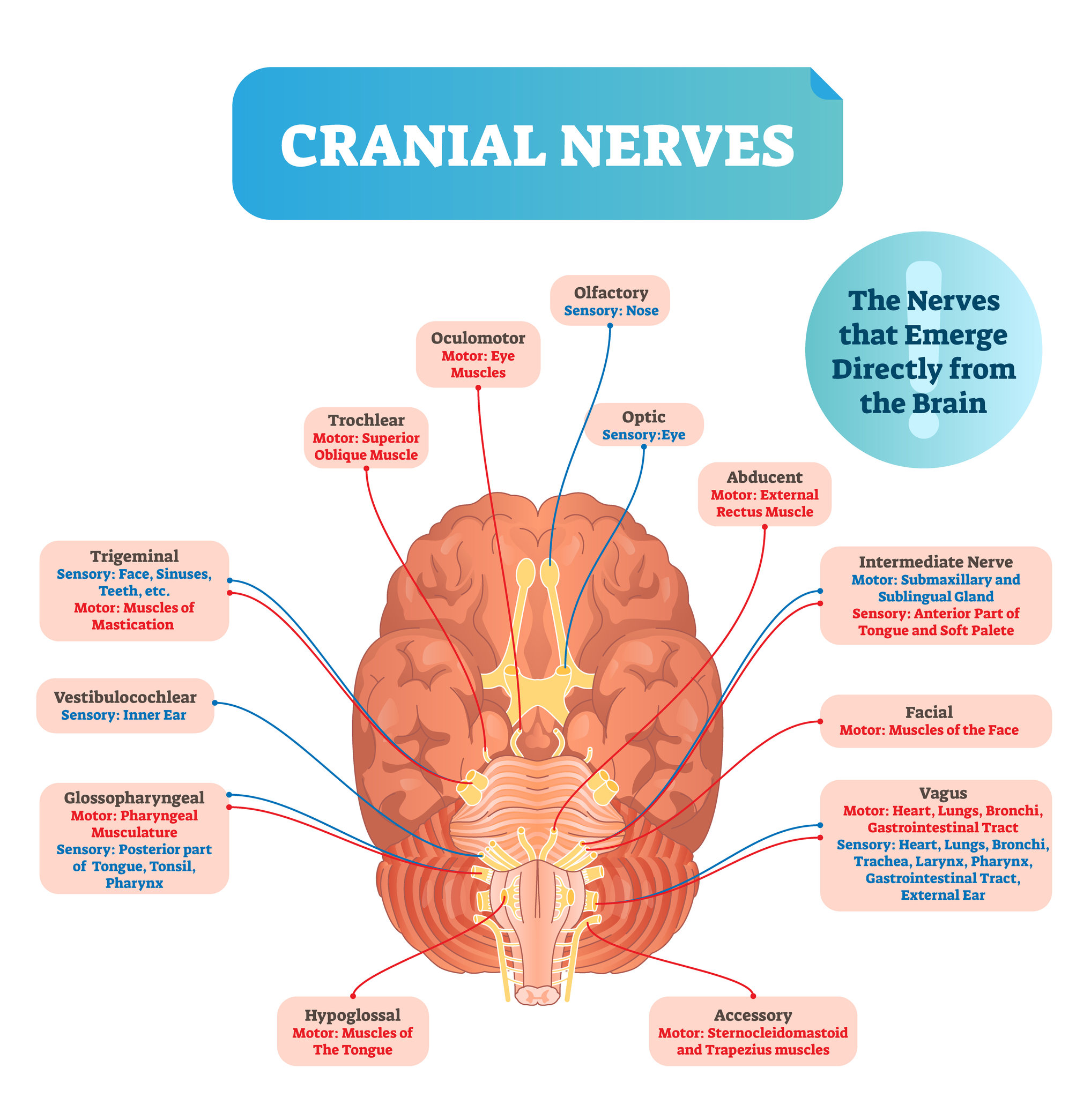
Most nerves exit the spinal cord in between vertebrae and travel to different parts of our body. But as you’ll see in the diagrams below, some nerves emerge directly from the brain without traveling through the spinal cord; these are the cranial nerves.
The cranial nerves are responsible for automatically controlling smooth muscles of organs as well as striated muscles in the head, neck, and trunk. They also receive sensation from these areas and send the sensory information back to the brain. The vagus nerve is the 10th cranial nerve.
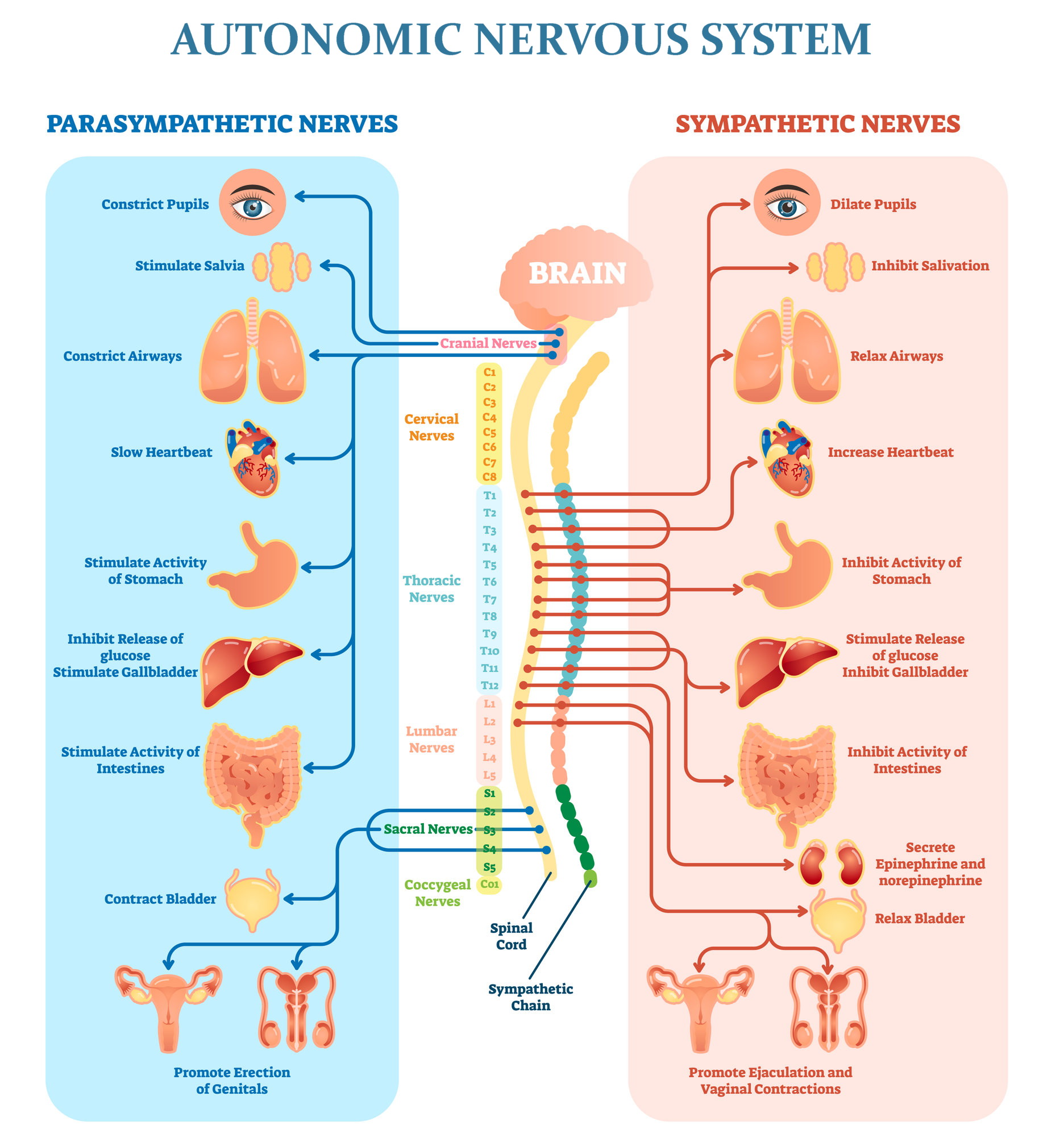
As shown in the diagram above, the Autonomic Nervous System (the part of our nervous system that controls our body automatically, without our conscious thought) is divided into the sympathetic and parasympathetic nervous systems. The sympathetic nervous system is in charge of the “fight or flight” response to stress when we perceive danger. The parasympathetic nervous system does the opposite: it calms us down, brings our body back into homeostasis, and allows for healing to occur.
The vagus nerve is the main neural component of the parasympathetic nervous system. It automatically controls parasympathetic motor functions of the heart, lungs, digestive system, liver, gallbladder, spleen, pancreas, and kidneys. This means that the vagus nerve has the very important job of stimulating the “rest and digest” functions of these organs.
The vagus nerve also controls striated skeletal muscles of the mouth, pharynx, and larynx, allowing us to swallow our food safely and speak.
While those are tremendous responsibilities, the nerve fibers that control all of those functions only make up about 20% of the fibers in the vagus nerve. The other 80% of vagal nerve fibers are afferent, meaning that they send sensory information from the organs back to the brain.
We can use this wealth of sensory information to tune into our body and notice when something feels not quite right. Often, the first sign of stress may be felt in the body instead of in our conscious awareness. Likewise, chronic stress can result in chronic physiological conditions. While we may be able to repress psychological issues, it’s hard to ignore a digestive problem or malfunctioning organ.
How the vagus nerve evolved
There are two sets of pathways within the vagal nerve. The first set of pathways is ancient and is shared with most vertebrates including reptiles. These nerve pathways are unmyelinated (lacking a protective myelin sheath), so their messages travel slowly.
These ancient unmyelinated pathways maintain homeostasis when the animal or person is in a safe situation. But when danger is detected, these pathways can trigger immobilization, slow the heart rate and metabolism, stop breathing, and even cause death.
Reptiles only have this first set of vagal pathways. But mammals evolved to have a second set of vagal pathways which are myelinated, so their messages travel more quickly.
In mammals, the older unmyelinated pathways mainly regulate organs below the diaphragm (digestive system, liver, gallbladder, spleen, pancreas, and kidneys). The newer myelinated pathways mainly regulate the heart and lungs, along with the striated skeletal muscles of the mouth, pharynx, and larynx. However, it’s important to note that if this newer set of vagal pathways is inhibited, enough of the older vagal pathways remain to initiate slowing and even stopping of the heart.
Why the sympathetic nervous system evolved
The sympathetic nervous system is in charge of the “fight or flight” response to stress when mammals perceive danger. The sympathetic nervous system prepares us for action by increasing heart rate and blood pressure, redirecting blood flow from the skin, stomach and intestines to the brain, heart and muscles, and making us breathe faster.
Reptiles’ main form of defense is the ancient vagal pathways that trigger immobilization. While reptiles are naturally adept at shifting back into homeostasis after being immobilized, mammals are not. We can’t survive long without adequate oxygen, so the sympathetic nervous system evolved in mammals as our main form of defense.
Based on the current understanding of how the Autonomic Nervous System evolved:
- The unmyelinated vagus nerve pathways developed first (these are the ancient pathways we share with reptiles)
- The sympathetic nervous system developed next, as mammals evolved from reptiles
- The myelinated vagus nerve pathways developed last; these play an important role in communicating with other mammals and maintaining homeostasis
All of the information we’ve covered so far is established neurobiology of the vagus nerve and Autonomic Nervous System. Now let’s learn about the Polyvagal Theory.
What is the Polyvagal Theory?
If you’ve ever read about the Polyvagal Theory, you may have felt confused—it’s complex, and Porges’ explanations of his theory are not simple or easy to understand. In a nutshell, Polyvagal Theory suggests that:
“When challenged, the regulation of the autonomic nervous system sequentially degrades to older circuits as an adaptive attempt to survive.” -Stephen Porges, The Pocket Guide to the Polyvagal Theory, p. 64
When we feel safe and there is no need to defend ourselves, the newest autonomic pathways—the myelinated vagus nerve pathways—are in charge. These pathways facilitate social interaction, growth, and recovery. They can also inhibit the older defense circuits from being triggered.
If we perceive danger, the sympathetic nervous system takes over and we go into fight-or-flight mode. In this state, both branches of the vagus nerve (new myelinated and old unmyelinated) are inhibited.
If our fight-or-flight defense mechanisms don’t make us feel safe, the sympathetic nervous system can become inhibited as the ancient unmyelinated vagus pathways take over. These pathways immobilize us and can make us faint.
When people experience chronic or repeated stress, they can get stuck in fight-or-flight mode. This can result in high blood pressure, elevated levels of stress hormones, anxiety, insomnia, and a host of other issues.
And when people experience trauma, their nervous system tends to shift into the most primitive form of defense—immobilization—and get stuck there. This can lead to a range of psychological problems including dissociation, avoidance, and the inability to communicate, as well as chronic physiological issues involving the organs of the body.
Mammals did not evolve to use this primitive form of defense on a regular basis—that’s what our sympathetic nervous system is for. So as I explained earlier, we are not good at shifting from immobilization back into homeostasis, because we didn’t evolve to have to do it often. When someone’s ancient vagal nerve pathways are activated, it’s very hard for their nervous system to move back into a state of feeling safe. Using what is known about the vagus nerve can allow clinicians to better help their patients who are stuck in this state of immobilization.
How we sense danger
There are two ways in which we sense danger: perception and neuroception. Perception requires our conscious awareness in order to detect cues that imply safety or danger. In contrast, neuroception (a term coined by Stephen Porges) describes how our nervous system automatically evaluates risk without our conscious awareness.
While we are not aware of the process of neuroception occurring in our subconscious, we may consciously notice our heart rate either slowing or speeding up, an uneasy feeling in our stomach, or other physiological changes that we associate with feeling safe or unsafe.
Remember how 80% of vagus nerve fibers are afferent, meaning they send sensory information from our body to our brain? Those nerve fibers go to the nucleus of the solitary track, located in the brain stem, letting our central nervous system know that our body has shifted into a different state.
‘When it comes to identifying safety from an adaptive survival perspective, the “wisdom” resides in our body and in the structures of our nervous system that function outside the realm of awareness…Cognitive evaluations of risk in the environment, including identifying potentially dangerous relationships, play a secondary role to our visceral reactions to people and places.’ -Porges, The Pocket Guide to Polyvagal Theory, p. 43
Porges makes the important note that our neuroception can sometimes be inaccurate. We may fail to detect danger, or we may detect danger when there is none. If we incorrectly sense danger, the older defense circuits can be triggered unnecessarily, and our nervous system can become stuck in fight-or-flight mode or immobilization.
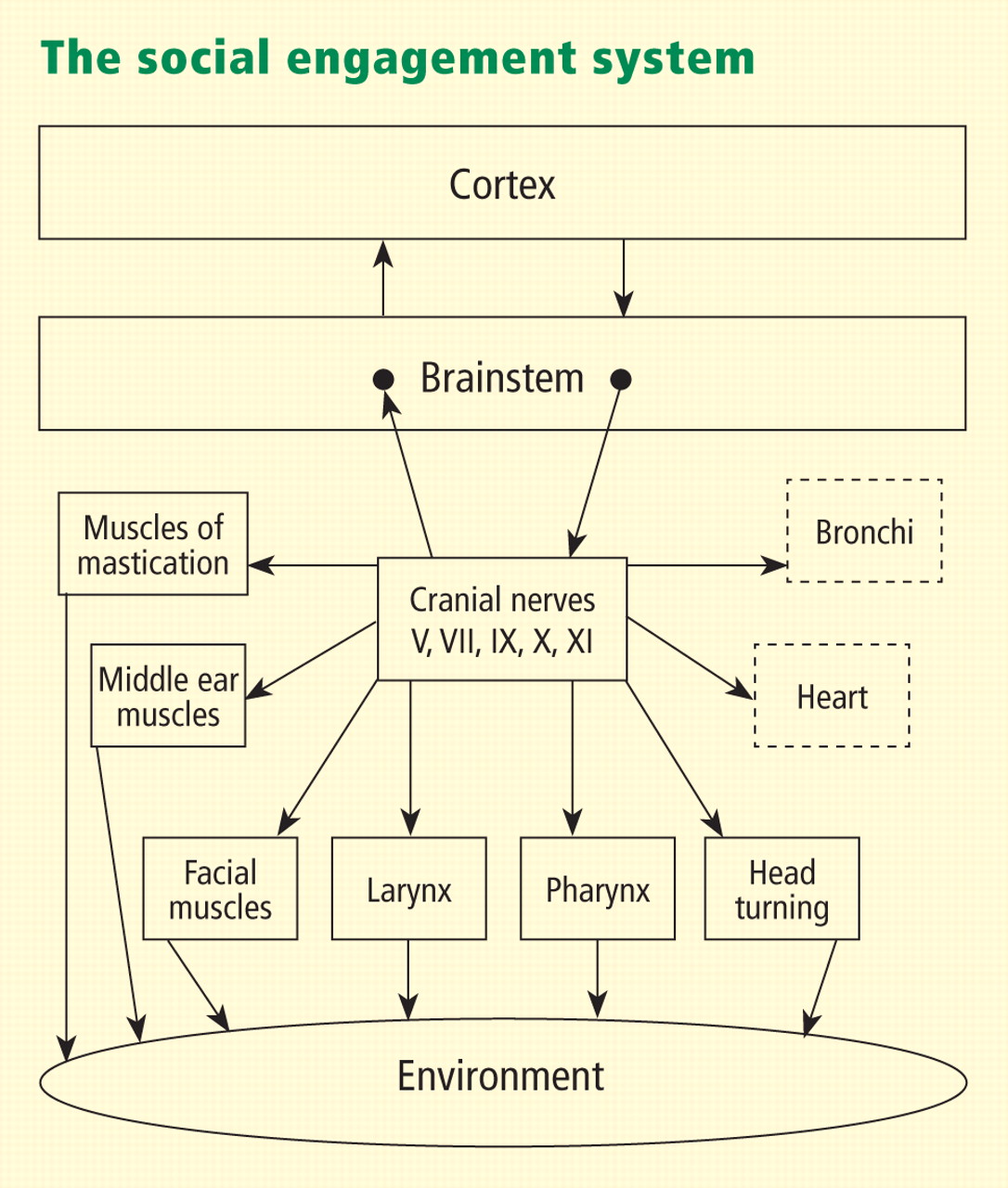
Communicating safety and danger with the Social Engagement System
The social engagement system is a network of motor pathways that control muscles of the face, head, heart, and lungs. The coordination and interaction of these neural pathways allow us to send facial expressions and bodily cues to other mammals. These signals let other mammals know whether or not we are safe to approach. The vagus nerve is one of the five cranial nerves involved in the social engagement system.
Reprinted from Biological Psychology (Porges SW. The polyvagal perspective. Biol Psychol 2007; 74:116–143), copyright 2007.
As mammals evolved, the social engagement system developed as a critical survival mechanism. By communicating with our social engagement system and sensing safety and danger with neuroception and perception, we’re able to live in groups harmoniously and communicate quickly and non-verbally.
Being able to live in groups is not only helpful, it is essential for mammals’ survival. We evolved to rely on others for sustenance and safety. We need to live in groups not only to secure food and protect ourselves physically, but also to co-regulate our physiological state. Co-regulation means that when we feel safe we give cues of safety to those around us, helping them to feel safe, and vice versa.
This is why being alone can be traumatic for mammals. As Porges writes, “To connect and co-regulate with others is our biological imperative. We experience this imperative as an inherent quest for safety that can be reached only through successful social relationships in which we co-regulate our behavior and physiology.”
We instinctively seek out connection and relationships with other humans and animals, particularly those who make us feel safe—unless our nervous system gets stuck in the ancient reptilian state of immobilization.
In next month’s post, I’ll discuss how Polyvagal Theory can be used in clinical settings to help people overcome the lasting effects of trauma.
Recommended reading:
The Pain Relief Secret: How to Retrain Your Nervous System, Heal Your Body, and Overcome Chronic Pain by Sarah Warren, CSE
Somatics: Reawakening the Mind’s Control of Movement, Flexibility and Health by Thomas Hanna