¿Qué es la inflamación crónica y por qué nos está matando?
Si parece que escuchas mucho sobre la inflamación, tienes razón. Se ha convertido en la última palabra de moda en el mundo de la salud debido a investigaciones que muestran el vínculo entre la inflamación y muchas afecciones crónicas, como cáncer, enfermedades cardíacas, diabetes, demencia y depresión. Desde que estas "enfermedades de la civilización" comenzaron a reemplazar a las enfermedades infecciosas, los investigadores han estado buscando un equivalente a la teoría de los gérmenes, el descubrimiento del siglo XIX que condujo a avances revolucionarios que incluyeron antibióticos, inmunización y pasteurización.
Durante 1990 sy principios 2000, comenzaron a acumularse investigaciones que demostraban el papel de la inflamación en enfermedades como el cáncer y la diabetes. A medida que el cuerpo de evidencia continúa creciendo, la comunidad médica ahora puede estar convergiendo en una teoría unificada de enfermedad crónica basada en el concepto de que la inflamación sistémica crónica de bajo grado es un factor subyacente y de mantenimiento en muchas toxinas relacionadas con el estilo de vida crónico condiciones inducidas.
En esta publicación, analizaré qué es la inflamación y cómo causa y contribuye al cáncer, la aterosclerosis y la diabetes tipo 2.
¿Qué es la inflamación?
Inflammation is part of our body’s natural, protective response to a dangerous invader (like a bacteria, virus, or toxin) or damage to our body’s own cells.
Our immune system does not discriminate between pathogenic or toxic invaders and physical trauma. Proteins called pattern recognition receptors detect both dangerous invaders and physical cell damage, and our immune system responds in the same way to both types of attacks.
Cuando se perciben estas amenazas a nuestra supervivencia, nuestro sistema inmunológico se acelera en su esfuerzo por eliminar los estímulos dañinos y comenzar el proceso de curación. En unos momentos, los vasos sanguíneos se dilatan y el aumento del flujo sanguíneo hace que el área de la lesión o infección se sienta caliente y parezca roja. Los capilares se vuelven permeables, lo que permite que los glóbulos blancos se muevan desde el torrente sanguíneo hasta el área lesionada. Esto causa hinchazón, lo que ayuda a aislar a los invasores o células dañadas del resto del cuerpo.
Las funciones de la respuesta inflamatoria son:
1. Aislar al peligroso invasor o células dañadas
2. Elimina las células muertas y otras sustancias dañinas.
3. Comience el proceso de reparación
Whenever I hear the word inflammation, I immediately translate that in my head to “immune system response.” This reminds me why it’s happening: because the body is in defense mode. If inflammation is occurring, that means that the cells in our body are detecting something that might be harmful to us.
Hay dos tipos diferentes de inflamación:
Localized inflammation occurs at the site of an injury or infection. A sprained ankle that is swollen and painful, or an infected cut that is red and swollen, are both examples of localized inflammation.
Systemic inflammation occurs throughout the body. This type of inflammation can be triggered by external sources including viral and bacterial infections, allergens or toxins in the food we eat and in our environment, smoking, and alcohol consumption. It can also be triggered by internal states including stress, obesity, autoimmune conditions, and genetic variations. (I’ll discuss why all of these things cause inflammation in an upcoming post!)
When localized or systemic inflammation is acute, or lasting just a few days, it is a good thing. We rely on this critical function of our immune system to heal our injuries and keep us protected from dangerous invaders.
Unfortunately, sometimes inflammation becomes chronic, lasting months or years. Inflammation can become chronic when the cause of inflammation continually occurs, when acute inflammation doesn’t resolve the situation, or when an autoimmune condition sets in.

"De las alas al centro del escenario: cómo la inflamación desencadena una multitud de enfermedades - Seminario de Longwood". Escuela Médica de Harvard. Transmitido en vivo en abril 18, 2017.
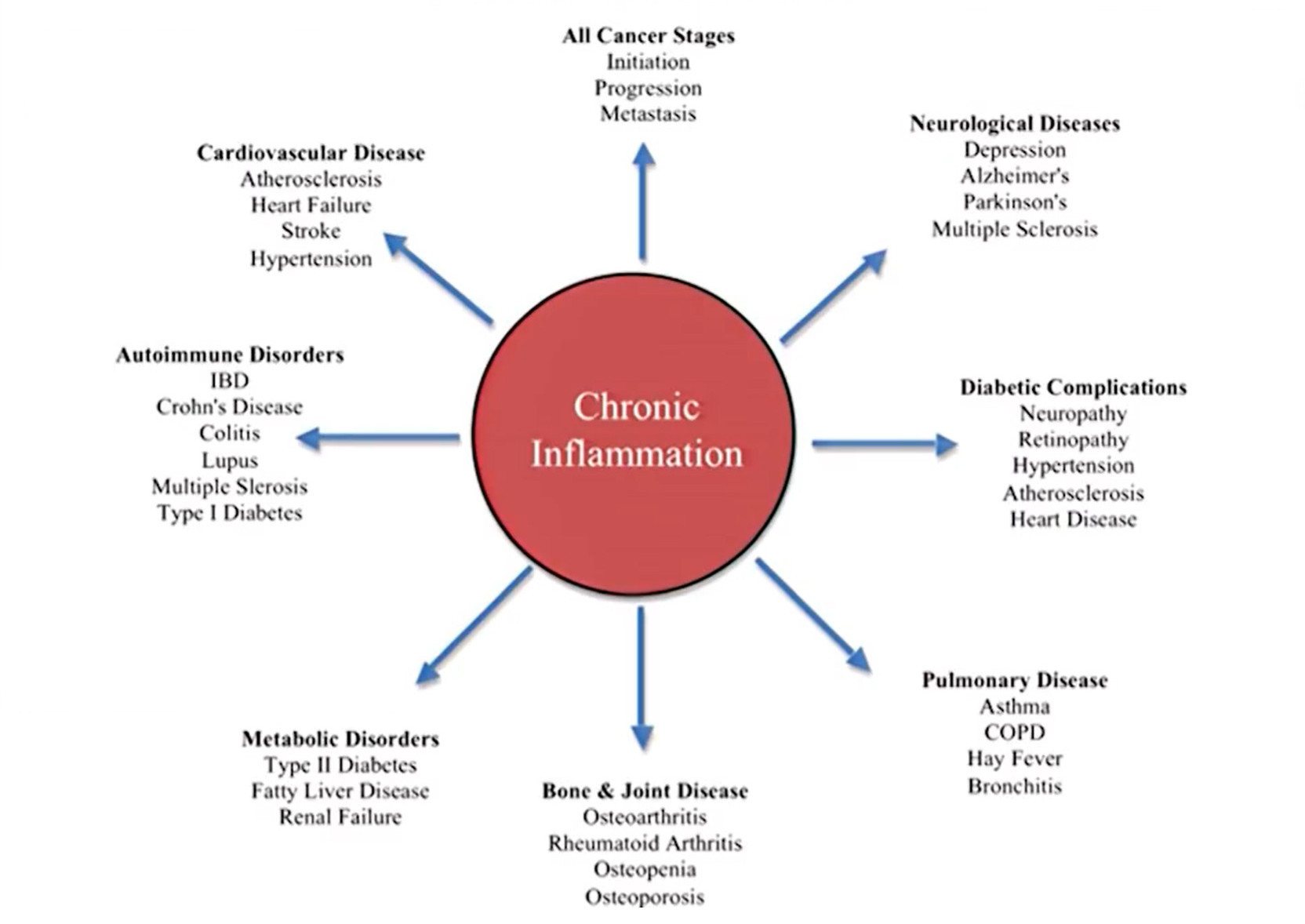
Our immune system evolved to expertly deal with short-term threats like injuries and infections. It did not evolve to deal with the never-ending barrage of threats that we now subject it to every day—like chronic stress, processed meat, and environmental toxins. As a result, chronic inflammation has many negative health effects and contributes to a wide range of health conditions (see chart below).
"De las alas al centro del escenario: cómo la inflamación desencadena una multitud de enfermedades - Seminario de Longwood". Escuela Médica de Harvard. Transmitido en vivo en abril 18, 2017.
Cómo la inflamación crónica causa y contribuye al cáncer
Cancer cells start out as normal, healthy cells. They become cancerous when their DNA (genetic material) mutates, or is altered. Cancer can start in any cell in the body.
While some people are born with genetic mutations that lead to cancer, these account for a small percentage of cancer cases. Most people get cancer due to genetic mutations that occur after birth. There are many causes of these gene mutations, including smoking, radiation, viruses, cancer-causing chemicals (carcinogens), obesity, hormones, alcohol consumption, lack of exercise, and chronic inflammation. It is estimated that up to 20% of cancers are related to chronic infections, 30% result from tobacco smoking and inhaled pollutants, and 35% are related to dietary factors, including obesity.
Las mutaciones genéticas más comunes que ocurren para crear células cancerosas son las que:
- Create rapid growth: A gene mutation can tell the cell to grow and divide more rapidly than normal; this creates many copies of this cell that all have the same mutation.
- Fail to stop cell growth: Normal cells have tumor suppressor genes that tell the cells when to stop growing, so that we don’t have too many of a certain type of cell. A mutation in a tumor suppressor gene allows cancer cells to keep growing and replicating.
- Alter DNA repair genes: Normal cells have DNA repair genes that repair errors in the cells’ DNA. A mutation in a DNA repair gene can allow errors to go uncorrected, leading the cell to become cancerous.
Now that we understand how and why normal cells become cancerous, let’s look at the two ways in which chronic systemic inflammation causes and contributes to cancer:
1. Chronic inflammation can cause the gene mutations in healthy cells that lead them to become cancerous. Research shows that gene mutations occur as a result of stress induced by the production of reactive oxygen and nitrogen species during the inflammatory process. Inflammation results in decreased expression of tumor suppressor genes and alteration of DNA repair pathways.
2. Cancer cells lure immune system cells into the tumor, resulting in tumor growth. The recruited immune system cells help to grow blood vessels within the tumor, contribute to cell growth within the tumor, and cause further gene mutations.
Now that the strong link between inflammation and cancer has been proven, research is showing how lifestyle modifications like a plant-based diet, exercise, and stopping smoking and alcohol consumption are effective in reducing inflammation and cancer risk. It has also been shown that anti-inflammatory drugs such as aspirin can reduce inflammation and cancer risk.
Cómo la inflamación crónica causa y contribuye a la aterosclerosis
Aterosclerosis is the buildup of plaques in arteries, also called hardening of the arteries. When these plaques rupture, they can cause blood clots, heart attacks, and strokes.
Como puede ver en la siguiente ilustración, las placas se acumulan en las paredes de las arterias debajo del endotelio, la delgada membrana que recubre el interior de las arterias. Las placas están compuestas de grasa, colesterol, calcio y otras sustancias que se encuentran en la sangre.

"De las alas al centro del escenario: cómo la inflamación desencadena una multitud de enfermedades - Seminario de Longwood". Escuela Médica de Harvard. Transmitido en vivo en abril 18, 2017.
Why do these plaques build up? Cholesterol has long been blamed for atherosclerosis, but high cholesterol levels alone may not be enough to cause plaques to form. In this 2011 study, researchers genetically modified mice so that the mice could not synthesize histamine, a compound that our bodies produce during inflammation and in response to stress. Without histamine, the mice did not form endothelial cell plaques—even though their blood cholesterol levels were high as a result of being fed a high-cholesterol diet. These results suggest that the histamine produced during our natural immune or stress response plays a critical role in atherosclerosis.
When plaques have formed, immune system cells migrate to the plaques and actually eat the cholesterol. The immune system cells get bigger and turn into foam cells which stay in place. They create waste, contribute to plaque buildup, and increase the risk of plaque rupture. In the illustration below, you can see how leukocytes (immune system cells) make up a large part of atherosclerotic plaques.

"De las alas al centro del escenario: cómo la inflamación desencadena una multitud de enfermedades - Seminario de Longwood". Escuela Médica de Harvard. Transmitido en vivo en abril 18, 2017.
La investigación muestra que los niveles altos de proteína C reactiva (PCR) en la sangre coinciden con tasas más altas de aterosclerosis; La PCR es un signo de inflamación que ocurre en el cuerpo. Y como era de esperar, los factores habituales relacionados con el estilo de vida que causan inflamación aumentan el riesgo de desarrollar aterosclerosis: tabaquismo, consumo de alcohol, estrés, obesidad, diabetes, una dieta poco saludable y falta de ejercicio.
Cómo la inflamación crónica causa y contribuye a la diabetes tipo 2
La diabetes ocurre cuando el nivel de glucosa (azúcar) en la sangre se vuelve demasiado alto. La glucosa en sangre es nuestra principal forma de energía y proviene de los alimentos que comemos. La insulina, una hormona producida por nuestro páncreas, permite que la glucosa se mueva desde nuestra sangre a nuestras células musculares para que pueda usarse como energía.
In type 2 diabetes, the body does not use insulin well (insulin resistance) or does not make enough insulin. As a result, glucose stays in the blood and builds up, leading to high blood glucose levels. Type 2 diabetes can develop at any age, and the greatest risk factor is body weight: about 87.5% of people with type 2 diabetes are overweight or obese.
As Dr. Michael Greger shows in this video, people eating a high-fat diet have higher levels of blood glucose than people eating a high-carbohydrate diet. Fat in the bloodstream can build up inside muscle cells, blocking insulin from doing its job of letting glucose into the muscle cells; this is how excess fat contributes to insulin resistance.
So, what role does inflammation play in insulin resistance? Researchers discovered that in people with type 2 diabetes, levels of pro-inflammatory cytokines (signaling proteins in the immune system) inside fat tissue are elevated. Their conclusion was that obesity-induced immune response contributes to insulin resistance. In other words, having excess body fat triggers inflammation in our body, which leads to a buildup of cytokines in fatty tissue, which prevents insulin from doing its job.
A second way in which inflammation contributes to type 2 diabetes is that once insulin resistance has developed, the insulin resistance itself can cause further inflammation. This can result in a vicious cycle in which inflammation causes insulin resistance and insulin resistance causes inflammation, leading to a continuous worsening of the condition.
Aproximadamente el 12.5% de las personas con diabetes tipo 2 no tienen sobrepeso, pero es probable que la inflamación también contribuya al desarrollo de la enfermedad. Algunas de estas personas tienen un peso corporal normal pero niveles altos de grasa visceral (grasa que crece alrededor de los órganos internos). Estas personas pueden sufrir la misma inflamación inducida por grasas que las personas con sobrepeso.
Smoking also causes inflammation in the body and is a significant risk factor for diabetes regardless of body weight. Chemicals in cigarette smoke injure cells, causing inflammation and preventing normal cell function.
People with chronic inflammatory diseases also have a higher risk of developing type 2 diabetes. About one-third of chronic hepatitis C patients develop type 2 diabetes, and people with rheumatoid arthritis have a 50% increased risk of developing type 2 diabetes.
Reducir el riesgo de desarrollar cáncer, aterosclerosis y diabetes tipo 2
Nuestra respuesta inmune natural nos permite recuperarnos de lesiones e infecciones, y no sobreviviríamos sin ella. Pero como ha aprendido, solo queremos que la inflamación se produzca cuando realmente la necesitemos, porque la inflamación crónica aumenta nuestro riesgo de desarrollar enfermedades mortales.
The good news is that many causes of chronic inflammation are lifestyle-related and entirely controllable. So while scientists develop new drugs and treatments aimed at reducing inflammation, the best way to prevent inflammation-related conditions is undeniably to live a healthy lifestyle and avoid chronic inflammation in the first place. Check out 12 Causes of Chronic Inflammation!

