Qu'est-ce que l'inflammation chronique et pourquoi tue-t-elle Us?
S'il semble que vous entendiez beaucoup parler d'inflammation, vous avez raison. C'est devenu le dernier mot à la mode dans le monde de la santé en raison de recherches montrant le lien entre l'inflammation et de nombreuses maladies chroniques, notamment le cancer, les maladies cardiaques, le diabète, la démence et la dépression. Depuis que ces « maladies de civilisation » ont commencé à remplacer les maladies infectieuses, les chercheurs ont cherché un équivalent à la théorie des germes - la découverte du XIXe siècle qui a conduit à des avancées révolutionnaires, notamment les antibiotiques, la vaccination et la pasteurisation.
Au cours des 1990 et du début des 2000, les recherches démontrant le rôle de l'inflammation dans des maladies telles que le cancer et le diabète ont commencé à s'accumuler. Alors que l'ensemble des preuves continue de croître, la communauté médicale pourrait maintenant converger vers une théorie unifiée des maladies chroniques basée sur le concept selon lequel l'inflammation systémique chronique de bas grade est un facteur sous-jacent et persistant dans de nombreuses maladies chroniques liées au mode de vie et aux toxines. conditions induites.
Dans cet article, je vais discuter de ce qu'est l'inflammation et comment elle cause et contribue au cancer, à l'athérosclérose et au diabète de type 2.
Qu'est-ce que l'inflammation ?
Inflammation is part of our body’s natural, protective response to a dangerous invader (like a bacteria, virus, or toxin) or damage to our body’s own cells.
Our immune system does not discriminate between pathogenic or toxic invaders and physical trauma. Proteins called pattern recognition receptors detect both dangerous invaders and physical cell damage, and our immune system responds in the same way to both types of attacks.
Lorsque ces menaces à notre survie sont perçues, notre système immunitaire passe à la vitesse supérieure dans ses efforts pour éliminer les stimuli nocifs et commencer le processus de guérison. En quelques instants, les vaisseaux sanguins se dilatent et l'augmentation du flux sanguin rend la zone de la blessure ou de l'infection chaude et rouge. Les capillaires deviennent perméables, permettant aux globules blancs de se déplacer de la circulation sanguine vers la zone lésée. Cela provoque un gonflement, ce qui aide à isoler les envahisseurs ou les cellules endommagées du reste du corps.
Les fonctions de la réponse inflammatoire sont de :
1. Isoler l'envahisseur dangereux ou les cellules endommagées
2. Éliminez les cellules mortes et autres substances nocives
3. Commencer le processus de réparation
Whenever I hear the word inflammation, I immediately translate that in my head to “immune system response.” This reminds me why it’s happening: because the body is in defense mode. If inflammation is occurring, that means that the cells in our body are detecting something that might be harmful to us.
Il existe deux types différents d'inflammation :
Localized inflammation occurs at the site of an injury or infection. A sprained ankle that is swollen and painful, or an infected cut that is red and swollen, are both examples of localized inflammation.
Systemic inflammation occurs throughout the body. This type of inflammation can be triggered by external sources including viral and bacterial infections, allergens or toxins in the food we eat and in our environment, smoking, and alcohol consumption. It can also be triggered by internal states including stress, obesity, autoimmune conditions, and genetic variations. (I’ll discuss why all of these things cause inflammation in an upcoming post!)
When localized or systemic inflammation is acute, or lasting just a few days, it is a good thing. We rely on this critical function of our immune system to heal our injuries and keep us protected from dangerous invaders.
Unfortunately, sometimes inflammation becomes chronic, lasting months or years. Inflammation can become chronic when the cause of inflammation continually occurs, when acute inflammation doesn’t resolve the situation, or when an autoimmune condition sets in.

"Des coulisses au centre de la scène : comment l'inflammation déclenche une multitude de maladies - Séminaire de Longwood." École de médecine de Harvard. Diffusé en direct sur avril 18, 2017.
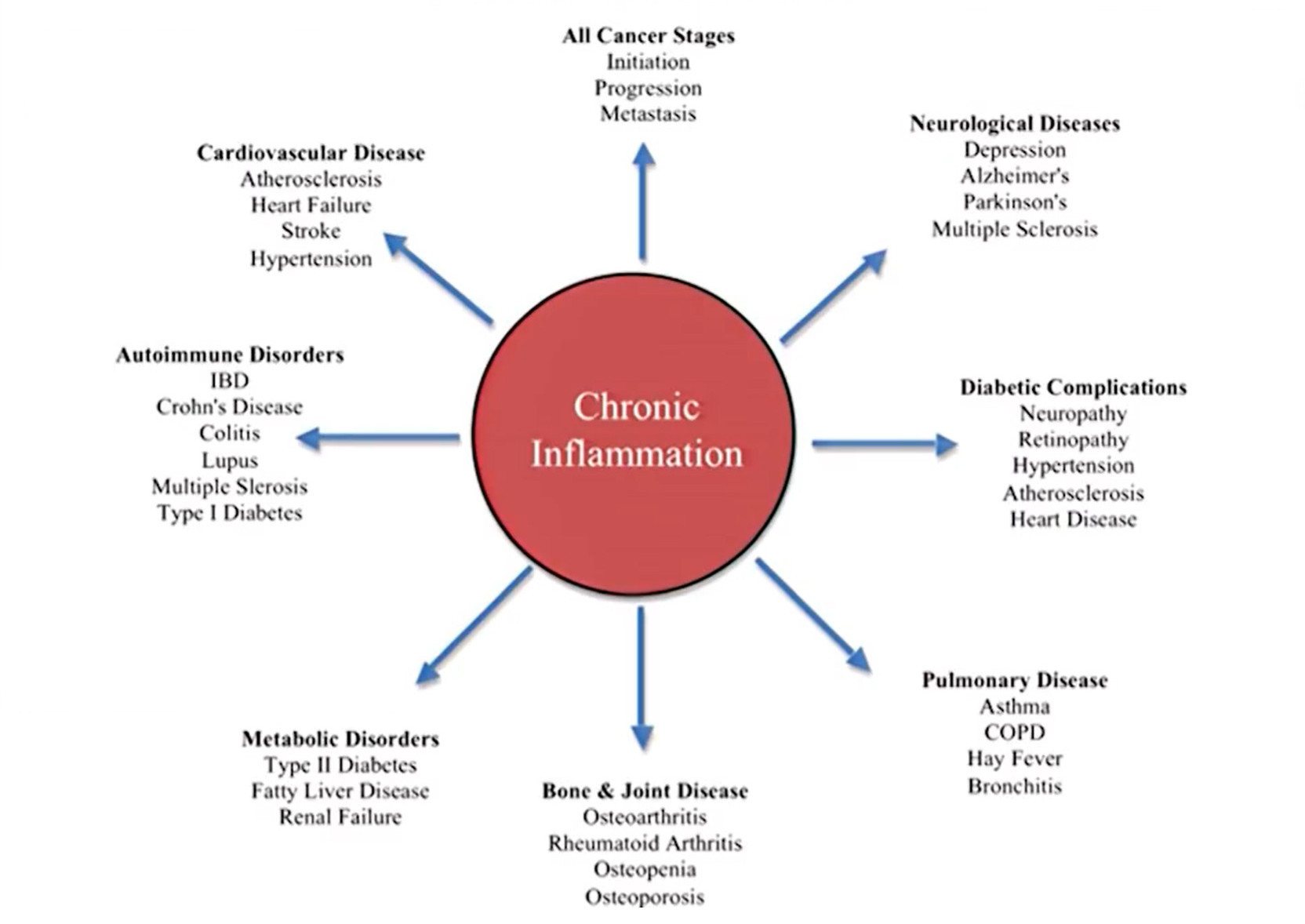
Our immune system evolved to expertly deal with short-term threats like injuries and infections. It did not evolve to deal with the never-ending barrage of threats that we now subject it to every day—like chronic stress, processed meat, and environmental toxins. As a result, chronic inflammation has many negative health effects and contributes to a wide range of health conditions (see chart below).
"Des coulisses au centre de la scène : comment l'inflammation déclenche une multitude de maladies - Séminaire de Longwood." École de médecine de Harvard. Diffusé en direct sur avril 18, 2017.
Comment l'inflammation chronique cause et contribue au cancer
Cancer cells start out as normal, healthy cells. They become cancerous when their DNA (genetic material) mutates, or is altered. Cancer can start in any cell in the body.
While some people are born with genetic mutations that lead to cancer, these account for a small percentage of cancer cases. Most people get cancer due to genetic mutations that occur after birth. There are many causes of these gene mutations, including smoking, radiation, viruses, cancer-causing chemicals (carcinogens), obesity, hormones, alcohol consumption, lack of exercise, and chronic inflammation. It is estimated that up to 20% of cancers are related to chronic infections, 30% result from tobacco smoking and inhaled pollutants, and 35% are related to dietary factors, including obesity.
Les mutations génétiques les plus courantes qui se produisent pour créer des cellules cancéreuses sont celles qui :
- Create rapid growth: A gene mutation can tell the cell to grow and divide more rapidly than normal; this creates many copies of this cell that all have the same mutation.
- Fail to stop cell growth: Normal cells have tumor suppressor genes that tell the cells when to stop growing, so that we don’t have too many of a certain type of cell. A mutation in a tumor suppressor gene allows cancer cells to keep growing and replicating.
- Alter DNA repair genes: Normal cells have DNA repair genes that repair errors in the cells’ DNA. A mutation in a DNA repair gene can allow errors to go uncorrected, leading the cell to become cancerous.
Now that we understand how and why normal cells become cancerous, let’s look at the two ways in which chronic systemic inflammation causes and contributes to cancer:
1. Chronic inflammation can cause the gene mutations in healthy cells that lead them to become cancerous. Research shows that gene mutations occur as a result of stress induced by the production of reactive oxygen and nitrogen species during the inflammatory process. Inflammation results in decreased expression of tumor suppressor genes and alteration of DNA repair pathways.
2. Cancer cells lure immune system cells into the tumor, resulting in tumor growth. The recruited immune system cells help to grow blood vessels within the tumor, contribute to cell growth within the tumor, and cause further gene mutations.
Now that the strong link between inflammation and cancer has been proven, research is showing how lifestyle modifications like a plant-based diet, exercise, and stopping smoking and alcohol consumption are effective in reducing inflammation and cancer risk. It has also been shown that anti-inflammatory drugs such as aspirin can reduce inflammation and cancer risk.
Comment l'inflammation chronique cause et contribue à l'athérosclérose
Athérosclérose is the buildup of plaques in arteries, also called hardening of the arteries. When these plaques rupture, they can cause blood clots, heart attacks, and strokes.
Comme vous pouvez le voir sur l'illustration ci-dessous, des plaques s'accumulent dans les parois des artères sous l'endothélium, la fine membrane qui tapisse l'intérieur des artères. Les plaques sont constituées de graisse, de cholestérol, de calcium et d'autres substances présentes dans le sang.

"Des coulisses au centre de la scène : comment l'inflammation déclenche une multitude de maladies - Séminaire de Longwood." École de médecine de Harvard. Diffusé en direct sur avril 18, 2017.
Why do these plaques build up? Cholesterol has long been blamed for atherosclerosis, but high cholesterol levels alone may not be enough to cause plaques to form. In this 2011 study, researchers genetically modified mice so that the mice could not synthesize histamine, a compound that our bodies produce during inflammation and in response to stress. Without histamine, the mice did not form endothelial cell plaques—even though their blood cholesterol levels were high as a result of being fed a high-cholesterol diet. These results suggest that the histamine produced during our natural immune or stress response plays a critical role in atherosclerosis.
When plaques have formed, immune system cells migrate to the plaques and actually eat the cholesterol. The immune system cells get bigger and turn into foam cells which stay in place. They create waste, contribute to plaque buildup, and increase the risk of plaque rupture. In the illustration below, you can see how leukocytes (immune system cells) make up a large part of atherosclerotic plaques.

"Des coulisses au centre de la scène : comment l'inflammation déclenche une multitude de maladies - Séminaire de Longwood." École de médecine de Harvard. Diffusé en direct sur avril 18, 2017.
La recherche montre que des niveaux élevés de protéine C-réactive (CRP) dans le sang coïncident avec des taux plus élevés d'athérosclérose; La CRP est un signe d'inflammation se produisant dans le corps. Et comme vous vous en doutez, les facteurs habituels liés au mode de vie qui causent l'inflammation augmentent le risque de développer l'athérosclérose : tabagisme, consommation d'alcool, stress, obésité, diabète, mauvaise alimentation et manque d'exercice.
Comment l'inflammation chronique cause et contribue au diabète de type 2
Le diabète survient lorsque le taux de glucose (sucre) dans le sang devient trop élevé. La glycémie est notre principale source d'énergie et elle provient des aliments que nous consommons. L'insuline, une hormone fabriquée par notre pancréas, permet au glucose de passer de notre sang à nos cellules musculaires afin qu'il puisse être utilisé comme source d'énergie.
In type 2 diabetes, the body does not use insulin well (insulin resistance) or does not make enough insulin. As a result, glucose stays in the blood and builds up, leading to high blood glucose levels. Type 2 diabetes can develop at any age, and the greatest risk factor is body weight: about 87.5% of people with type 2 diabetes are overweight or obese.
As Dr. Michael Greger shows in this video, people eating a high-fat diet have higher levels of blood glucose than people eating a high-carbohydrate diet. Fat in the bloodstream can build up inside muscle cells, blocking insulin from doing its job of letting glucose into the muscle cells; this is how excess fat contributes to insulin resistance.
So, what role does inflammation play in insulin resistance? Researchers discovered that in people with type 2 diabetes, levels of pro-inflammatory cytokines (signaling proteins in the immune system) inside fat tissue are elevated. Their conclusion was that obesity-induced immune response contributes to insulin resistance. In other words, having excess body fat triggers inflammation in our body, which leads to a buildup of cytokines in fatty tissue, which prevents insulin from doing its job.
A second way in which inflammation contributes to type 2 diabetes is that once insulin resistance has developed, the insulin resistance itself can cause further inflammation. This can result in a vicious cycle in which inflammation causes insulin resistance and insulin resistance causes inflammation, leading to a continuous worsening of the condition.
Environ 12.5 % des personnes atteintes de diabète de type 2 ne sont pas en surpoids, mais l'inflammation contribue probablement également au développement de la maladie. Certaines de ces personnes ont un poids corporel normal mais des niveaux élevés de graisse viscérale (graisse qui se développe autour des organes internes). Ces personnes peuvent souffrir de la même inflammation induite par les graisses que les personnes en surpoids.
Smoking also causes inflammation in the body and is a significant risk factor for diabetes regardless of body weight. Chemicals in cigarette smoke injure cells, causing inflammation and preventing normal cell function.
People with chronic inflammatory diseases also have a higher risk of developing type 2 diabetes. About one-third of chronic hepatitis C patients develop type 2 diabetes, and people with rheumatoid arthritis have a 50% increased risk of developing type 2 diabetes.
Réduire votre risque de développer un cancer, une athérosclérose et un diabète de type 2
Notre réponse immunitaire naturelle permet us pour se remettre de blessures et d'infections, et nous ne survivrions pas sans cela. Mais comme vous l'avez appris, nous voulons que l'inflammation ne se produise que lorsque nous en avons vraiment besoin, car l'inflammation chronique augmente notre risque de développer des problèmes de santé mortels.
The good news is that many causes of chronic inflammation are lifestyle-related and entirely controllable. So while scientists develop new drugs and treatments aimed at reducing inflammation, the best way to prevent inflammation-related conditions is undeniably to live a healthy lifestyle and avoid chronic inflammation in the first place. Check out 12 Causes of Chronic Inflammation!

