L'exercice forcé et la réduction du stress inversent les symptômes de la maladie de Parkinson
If you read last week’s post Doctors Call for an End to the Parkinson’s Pandemic, you learned that Parkinson’s disease is most often the result of a complex interplay between genetic and environmental factors, which include exposure to neurotoxic chemicals, head trauma, lack of exercise, diet, gut dysbiosis, and chronic stress.
Bien qu'il n'y ait pas de remède pour la maladie de Parkinson, il existe des cas documentés d'amélioration et de rétablissement. La récupération dans ces cas est définie principalement par une élimination des symptômes moteurs. Comme je l'ai mentionné dans l'article de la semaine dernière, les symptômes moteurs commencent lorsque les niveaux de dopamine et la perte de neurones atteignent un seuil critique. J'expliquerai comment cela fonctionne dans cet article. Lorsque les personnes sont capables d'augmenter leur taux de dopamine et/ou de restaurer suffisamment de neurones dopaminergiques pour dépasser ce seuil, leurs symptômes moteurs peuvent disparaître.
Dans cet article, je vais discuter de la raison pour laquelle les symptômes moteurs se produisent, de la recherche sur la neurogenèse dans la substantia nigra des patients atteints de la maladie de Parkinson, de la façon dont l'exercice (en particulier l'exercice forcé) et la réduction du stress réduisent les symptômes moteurs, et des histoires de guérison de la maladie de Parkinson. Comme vous l'apprendrez, la réduction et potentiellement l'élimination des symptômes moteurs, et même la restauration de l'odorat, est un objectif réaliste que les patients atteints de la maladie de Parkinson poursuivent déjà.
Les symptômes moteurs surviennent lorsque la voie « NoGo » est activée
The motor symptoms of Parkinson’s disease typically appear years after the disease process has begun—often 20 or more years after. It’s estimated that motor symptoms appear when approximately 30% to 60% of dopaminergic (dopamine-producing) neurons in the substantia nigra are lost. Studies show varied results when it comes to the actual percentage of substantia nigra neuron loss necessary to produce motor symptoms, and it’s safe to say that the exact percentage is different from person to person. Regardless of the percentage, it is understood that when dopamine levels decrease to a critical threshold, tremor or other motor symptoms may be felt—sometimes suddenly. For many people, this is the first noticeable sign of the disease.
Dopaminergic neurons in the substantia nigra send dopamine into two basal ganglia motor loops, referred to as the direct pathway of movement and the indirect pathway of movement. Dopamine regulates motor activity by acting on dopamine receptors, of which there are two types: D1-like receptors are present in the direct pathway, and D2-like receptors are present in the indirect pathway (if you read more about this topic, you’ll hear about these receptors).
The direct pathway allows us to move in ways that we want to; activation of the direct pathway increases ease of movement and of initiating movement. In contrast, the indirect pathway allows us to suppress unwanted movement.
The direct pathway is referred to as the “Go” pathway, while the indirect pathway is referred to as the “NoGo” pathway. When the Go pathway is activated, we move easily; when the NoGo pathway is activated, movement is suppressed.
Low or fluctuating levels of dopamine, which occur in Parkinson’s disease as dopaminergic neurons die off, weaken the direct pathway and strengthen the indirect pathway. When dopamine levels fall to a critical threshold, tremor or other motor symptoms may occur, sometimes suddenly, as the indirect pathway is activated.
Neurogenèse dans la substantia nigra et traitements prometteurs par cellules souches
In last week’s post I explained that Parkinson’s disease is a degenerative neurological condition in which dopaminergic (dopamine-producing) neurons in a part of the brain called the substantia nigra die off. Other parts of the brain suffer neurodegeneration as well, causing some of the non-motor symptoms of Parkinson’s. I’ll now discuss promising research about neurogenesis (production of new neurons) as it applies to Parkinson’s disease; if you’re not familiar with neurogenesis, I encourage you to read this post.
In 2003, scientists in Sweden demonstrated that neurogenesis occurs in the substantia nigra of adult mice. Their research showed that the type of dopaminergic neurons lost in Parkinson’s disease are actually regenerated throughout life. While the rate of neurogenesis in the substantia nigra is slower than in the hippocampus, if the rate of neural turnover is constant, the entire population of dopaminergic neurons in the substantia nigra could be replaced during the lifespan of a mouse. The study showed that not only does neurogenesis in the substantia nigra occur, but the newborn neurons are then integrated into neural circuits.
Les découvertes de cette étude impliquent que "des perturbations dans l'équilibre finement réglé de la genèse cellulaire et de la mort cellulaire pourraient entraîner des troubles neurodégénératifs". Les chercheurs suggèrent que la maladie de Parkinson pourrait dans certains cas être causée par une diminution de la neurogenèse plutôt que par une augmentation de la mort cellulaire. Une autre explication qu'ils suggèrent est que la neurogenèse chez les patients atteints de la maladie de Parkinson ne peut pas suivre le taux accru de mort cellulaire causée par les corps de Lewy.
In 2016, researchers at Boise State University in Idaho discovered that dopaminergic neurons are replenished in adult mouse models of Parkinson’s disease. The researchers created a chronic, systemic inflammatory state in mice’s brains to simulate that which occurs in Parkinson’s disease. Their results indicate that inflammation may inhibit neurogenesis in the substantia nigra, leading or contributing to the net loss of neurons in Parkinson’s disease. The researchers note that neurogenesis has been difficult to prove due to limitations of current cell lineage tracing methods, and they were able to demonstrate neurogenesis of nigral neurons using a new tracing model that they developed.
In 2011, neuroscientists in the Netherlands studied the brains of 25 people: 10 with Parkinson’s disease, 10 healthy controls, and 5 with Lewy body disease (the presence of Lewy bodies, but no clinical symptoms of Parkinson’s disease). The researchers found neural stem cells in the subventricular zone of every donor, with no significant differences in number between the three groups. They cultured neural stem cells from the Parkinson’s patients and confirmed that the cells were viable. While this was a small study, having proof that viable neural stem cells are produced in the brains of Parkinson’s patients is extremely encouraging.
An article in the Journal of Experimental Neuroscience states: “To compensate the degenerative rate of DAergic neurons, we have only 2 choices, either enhance the formation of newborn neurons and endogenous regenerative capacity or reduce the death rate of existing neurons.” Many scientists are pursuing the first route—exploring ways to enhance our natural process of producing neural stem cells to replace the dopaminergic neurons that are lost in Parkinson’s disease.
In 2012, researchers in South Korea injected human stem cells into mice with Parkinson’s disease. The stem cells increased neurogenesis in the subventricular zone and the substantia nigra, which led to an increase in the number of neural precursor cells that turned into dopaminergic neurons in the substantia nigra. The researchers suggest that this approach of enhancing endogenous neurogenesis to repair the damaged Parkinson’s brain could have a significant impact on future strategies.
However, scientists in the Netherlands and Australia favor non-invasive approaches. They caution that transplanting neural stem cells has both ethical and immunological challenges. When doing stem cell transplants, a donor is necessary, and the patient’s immune system must be suppressed in order to prevent rejection. These scientists prefer non-invasive treatment approaches that stimulate neurogenesis and mobilize endogenous neural stem cells—those that are naturally produced in the brain—to survive, migrate, and differentiate into dopaminergic neurons in the substantia nigra.
One such approach is being explored by neuroscientists at the Karolinska Institute in Sweden. By injecting transcription factors (proteins that regulate genes) into mice with Parkinson’s, they can turn astrocytes (an abundant type of brain cell that provide support and maintain homeostasis) into dopaminergic neurons. Five weeks after receiving treatment, the mice with Parkinson’s were walking normally. This “direct reprogramming of brain cells has the potential to become a novel therapeutic approach for Parkinson’s.”
L'un des auteurs de l'étude note que les cellules reprogrammées seraient probablement endommagées par ce qui a causé la maladie de Parkinson en premier lieu. Dans les greffes de cellules pour d'autres problèmes de santé, la maladie a tendance à rattraper les cellules transplantées en 15-20 ans. Les traitements visant à améliorer la neurogenèse endogène feront probablement gagner un temps important aux patients atteints de la maladie de Parkinson, mais ils devront peut-être être répétés.
Jusqu'à et même après que ces traitements soient approuvés pour un usage humain, il est extrêmement important pour les patients atteints de la maladie de Parkinson de comprendre comment améliorer naturellement la neurogenèse. L'exercice et la réduction du stress sont deux des meilleurs moyens d'encourager les cellules souches neurales à survivre, à migrer et à se différencier en le type de neurones dont le cerveau a besoin. Les patients atteints de la maladie de Parkinson utilisent déjà l'exercice et la réduction du stress pour réparer leur cerveau endommagé, et le résultat est une réduction ou une élimination des symptômes moteurs, et même une restauration de l'odorat.
Pour les patients atteints de la maladie de Parkinson, l'exercice fait ce que les médicaments ne peuvent pas
We learned last week that exercising regularly helps to prevent Parkinson’s. In a study of more than 7,300 male veterans, those with the lowest level of physical fitness had a 316% higher risk of developing Parkinson’s than those with the highest level of physical fitness. And a meta-analysis of more than half a million participants found a dose-response relationship: The more moderate to vigorous physical activity you do, the more your risk of getting Parkinson’s is reduced.
Reduced physical activity is likely an early symptom of Parkinson’s disease. But neuroscientists at the University of Texas in Austin did an interesting study to explore whether or not a reduction in physical activity also speeds up the degeneration of dopaminergic neurons. By restricting the movement of rats, they were able to show that the restriction of movement led to severe and chronic loss of dopaminergic neurons and impaired motor function. Neurons that aren’t used tend to wither away and die—this is called neural pruning. When it comes to movement, the principle of “use it or lose it” applies not only to our muscles, but to the health of our brain as well.
Nous savons donc que l'exercice protège contre la maladie de Parkinson, c'est formidable. Si vous faites déjà de l'exercice, continuez à le faire et si vous ne le faites pas, commencez. Mais qu'en est-il si vous avez déjà la maladie de Parkinson ?
A 2017 study at the Cleveland Clinic in Ohio had exciting results. Using fMRI scans, researchers found that forced exercise (which I’ll describe in the next section) and Parkinson’s medications had very similar effects on the brain. Forced exercise also improved participants’ scores on the Unified Parkinson’s Disease Rating Motor Scale by 50%. The researchers explain that “Both levodopa therapy and forced exercise are thought to increase the amount of available dopamine within the dorsolateral striatum.” They also note that exercise has little expense and none of the negative side effects of medication that can compromise quality of life for Parkinson’s patients.
Likewise, a team of researchers from the U.S., China, and Spain agree that “exercise is a universally available, side effect-free medicine that should be prescribed to vulnerable populations as a preventive measure and to Parkinson’s disease patients as a component of treatment.” They note that there is currently no pharmacological treatment that can modify or slow the disease or protect dopaminergic neurons—for Parkinson’s patients, exercise does what medication can’t.
The main way that exercise stimulates neurogenesis and keeps the brain healthy is by boosting production of neuroprotective growth factors, one of which is brain-derived neurotrophic factor (BDNF). BDNF is a protein that acts like Miracle-Gro for brain cells: it stimulates the growth of new neurons, helps them survive, and encourages the formation of new synapses. Neurotrophic factors increase neurogenesis in the substantia nigra, and may help to recover the phenotype of dopaminergic neurons or increase sprouting of dopaminergic axons. Studies have also shown that exercise reduces damage to dopaminergic neurons in motor circuits, preserves dopamine levels in Parkinson’s animal models, and reduces cellular inflammation and oxidative stress.
Parkinson’s patients who exercise more than 3 times per week for a total of more than 180 minutes have a more robust dopamine system and more dopamine release in response to exercise when compared to Parkinson’s patients who exercise less often or for shorter durations. They also experience less bradykinesia, better function, and less apathy.
Running can completely protect mice from the neurotoxic effects of MPTP, a chemical that kills dopaminergic neurons in the substantia nigra, causing Parkinson’s disease. Researchers found that one month of voluntary running on a running wheel provided no protection, two months provided partial protection, and three months provided complete protection of loss of dopaminergic neurons.
In addition to protecting against the loss of neurons, running has been shown to increase the number of dopaminergic neurons in animal models of Parkinson’s. Researchers observed restoration of lost neurons after 18 weeks of treadmill running in mice treated with MPTP. And researchers in Korea found that running for 30 minutes twice a day for just 16 days was enough to recover some of the dopaminergic neurons killed by the neurotoxin 6-OHDA.
Le Dr Jay Alberts découvre la magie de l'exercice forcé pour les patients atteints de la maladie de Parkinson
In 2003 Dr. Jay Alberts rode the Des Moines Register’s Annual Great Bike Race Across Iowa with his friend Cathy, who has Parkinson’s disease. Dr. Alberts rode the front of a tandem bicycle with Cathy pedaling behind him. Cathy remarked, “for this week it did not feel like I had Parkinson’s.” After several days of riding, Dr. Alberts noticed that Cathy’s motor control, most notably her handwriting, had improved. This set him on a path toward groundbreaking research on the benefits of forced exercise for Parkinson’s patients.
When the effects of exercise are tested in animal models of Parkinson’s, the exercise is often “forced,” meaning that the animal is forced to exercise at a more intense level than they would choose to on their own. Researchers have found that this forced exercise (FE) is far more effective than voluntary exercise in stimulating the release of neurotrophic factors and enhancing neurogenesis. Researchers suggest that “contradictory results in human and animal studies are caused by differences between voluntary (human) versus forced exercise (animal)…patients with PD may not be able to exercise (voluntarily) at sufficiently high rates to trigger the endogenous release of the neurotrophic factors thought to underlie global improvements in motor function.”
Dr. Alberts realized that in riding on the back of a tandem bike with him, Cathy was doing forced exercise—pedaling faster than she would have on her own. So in 2009, he and other researchers at the Cleveland Clinic tested the effects of forced exercise versus voluntary exercise for Parkinson’s patients. Patients completed eight weeks of either forced exercise or voluntary exercise on stationary bicycles. Patients in the forced exercise group were forced to pedal at a speed 30% faster than their preferred voluntary speed. While cardiovascular fitness improved for both groups, the forced exercise group showed a 35% improvement in motor function, while the voluntary exercise group had no improvement.
Un aspect passionnant des résultats de l'étude était le fait que, alors que l'exercice forcé n'utilisait que les muscles du bas du corps, le contrôle moteur s'améliorait dans les tâches de dextérité manuelle utilisant le haut du corps. Cela signifiait que l'exercice forcé n'améliorait pas seulement le contrôle musculaire ou la force localement dans les muscles qui étaient exercés ; il améliorait la fonction motrice en affectant le cerveau d'une manière ou d'une autre.
And remarkably, three participants in the study noticed that their sense of smell had returned. One noted that he could smell diesel fuel for the first time in 10 years, another walked into his house and smelled onions, and the third suddenly realized that he had body odor. These observations led the researchers to start tracking improvements in olfaction (sense of smell), the loss of which is often a very early symptom of Parkinson’s. They found that improvements in sense of smell correlated with pedaling speed; participants who pedaled faster than 83 RPM tended to have improvements in olfaction.
Dr. Alberts and his team then carried out a study which I mentioned earlier. In this study, forced exercise improved motor function by 50%. The researchers used fMRI scans to see how exercise affected the participants’ brains, and as you can see below, they found that forced exercise and medication activate the same brain areas. The researchers explain: “Both levodopa therapy and forced exercise are thought to increase the amount of available dopamine within the dorsolateral striatum.”
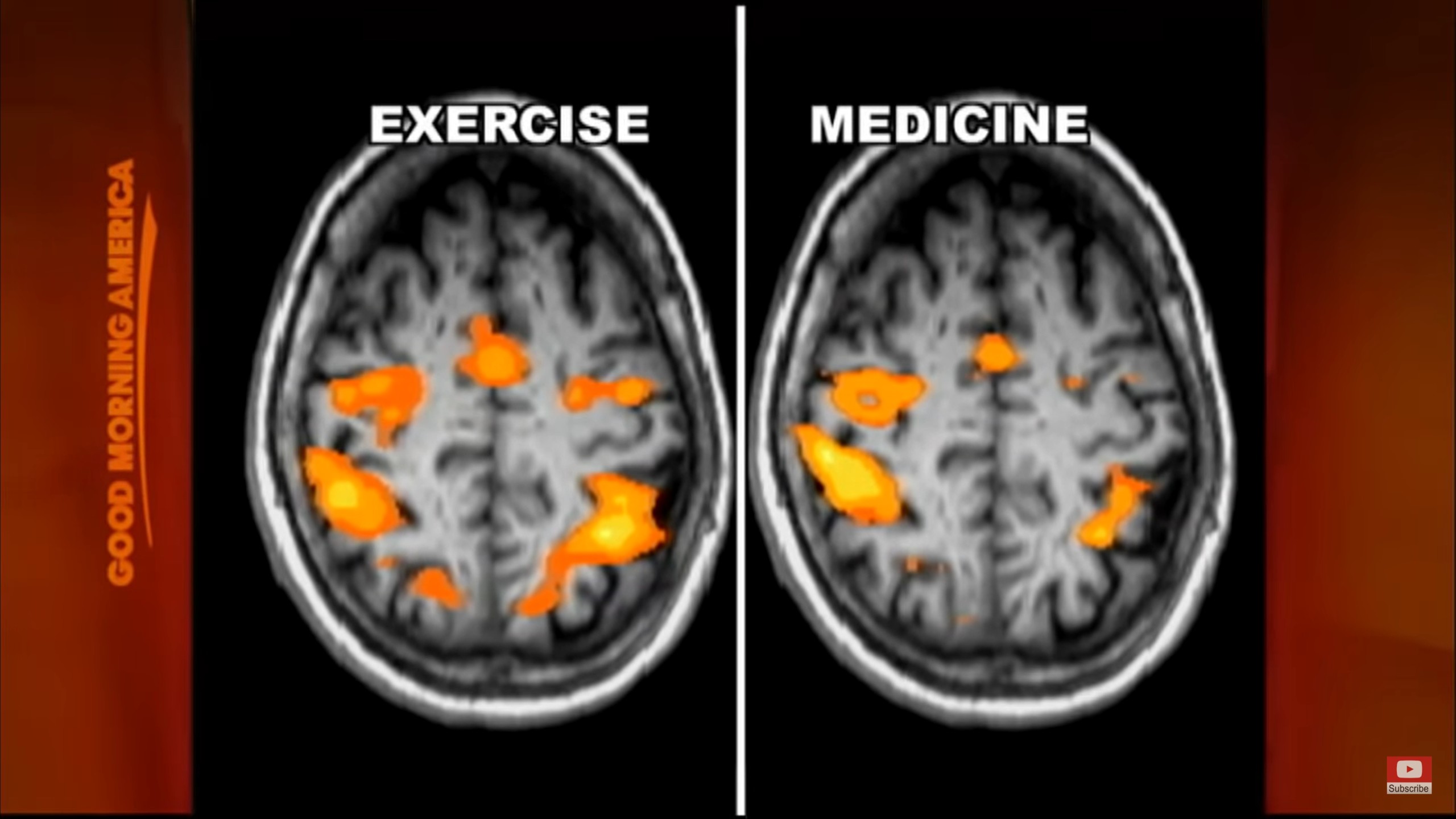
From Good Morning America.
Dr. Alberts and his team then carried out a trial with 100 Parkinson’s patients. They found that “an 8-week high intensity aerobic exercise program significantly improved motor function scores, turning and gait speed, and information processing.” And somewhat surprisingly, the positive results continued for up to eight weeks after the participants stopped exercising, showing that the exercise had led to lasting changes in brain function.
En mai 2019, le Dr Alberts a reçu une subvention de 3 millions de dollars sur cinq ans pour mener un essai clinique étudiant les effets à long terme de l'exercice aérobique de haute intensité sur la maladie de Parkinson. L'essai suivra les progrès de 250 patients atteints de la maladie de Parkinson alors qu'ils participent au programme d'exercices pendant une année complète. C'est très excitant parce que les essais précédents, ainsi que d'autres études d'interventions pour la maladie de Parkinson, ont généralement été réalisés sur des périodes de temps très courtes. Lorsqu'il s'agit d'une maladie en cours depuis des décennies, tester une intervention pendant seulement huit semaines est limitant.
Participants in this latest study use Peloton indoor bikes at home, are instructed to exercise three times per week for 12 months, and have their motor function evaluated every three months throughout the year. The study is in its first year right now, recruitment of participants is ongoing, and results may be published within the next few years. The researchers hope this will lead to patient-specific exercise prescriptions that take into account individual disease variables and can estimate potential outcomes. Since forced exercise has comparable effects as medications and deep brain stimulation on improving motor function, Dr. Alberts says “exercise is medicine” for Parkinson’s patients.
If you’re interested in this topic, you may enjoy watching Dr. Alberts describe his research in a talk he gave for the Davis Phinney Foundation for Parkinson’s. Dr. Alberts makes a number of important points, one of which is that when doing forced exercise on a tandem bicycle, the Parkinson’s patient must be actively involved and contributing to the movement. If the patient is passive, they do not experience improvement in motor function.
De plus, l'exercice ne doit pas nécessairement être du vélo. Le Dr Alberts suggère qu'un tapis roulant ou un rameur stationnaire pourrait également être utilisé - l'aspect le plus important de l'exercice est que la personne doit s'entraîner à un rythme plus rapide qu'elle ne le ferait par elle-même. Il recommande de réduire la résistance afin d'augmenter la vitesse.
Dr. Alberts and Cathy Frazier, his friend whose experience first inspired his research, created Pedaling for Parkinson’s, a group indoor cycling class that is now held all over the country. If you’re interested in trying this approach, check to see if there’s a Pedaling for Parkinson’s class near you!
Dr. Alberts appears in the documentary Ride with Larry, an inspiring film that follows Parkinson’s patient Larry Smith as he does a 300-mile bike ride across South Dakota. The film also offers a helpful introduction to the use of medical marijuana, which Larry finds very helpful in relieving his Parkinson’s symptoms.
A final note on exercise: Vigorous, forced exercise is not the only type of exercise that Parkinson’s patients should do; they can also benefit greatly from types of movement that involve building strength, coordination, and balance. For example, yoga improves motor function, postural stability, functional gait and freezing gait, and reduces the risk of falling in Parkinson’s patients. Similarly, Tai Chi reduces risk of falling and improves motor function in Parkinson’s patients.
Practicing forced aerobic exercise in addition to other types of movement that you enjoy is an ideal combination. Dr. John Ratey, author of Spark: The Revolutionary New Science of Exercise and the Brain, recommends doing both aerobic exercise and activities that demand focus and coordination, like martial arts, dance, rock climbing, and yoga, in order to fully stimulate your brain.
La pleine conscience, la méditation et la réduction du stress réduisent les symptômes de la maladie de Parkinson et stimulent la dopamine
If you read last week’s post, you learned why chronic stress is a risk factor for Parkinson’s disease. Chronic stress causes neuroinflammation, oxidative stress, and elevated cortisol levels, which lead to a loss of dopaminergic neurons in the substantia nigra. Chronic stress also decreases neurogenesis. Stressful life events, job-related stress, and stress-related personality traits all increase the risk of developing Parkinson’s. Stress level also worsens motor symptoms and predicts worse disease progression.
The idea that chronic stress is a factor in developing Parkinson’s has become mainstream fairly recently. Studies have shown how stress leads to the death of dopaminergic neurons, but not much research has been done yet to test how methods of stress reduction may improve symptoms, and those that have been done have been short-term. However, in personal reports of improvement of motor symptoms and recovery, nearly everyone cites mindfulness, mindful movement, meditation, and/or stress reduction as a critical part of their recovery—you’ll read some of these stories in the next section.
In 2013, scientists in Belgium carried out the first study to test the neurobiological effects of mindfulness in Parkinson’s patients. After eight weeks of a mindfulness practice, the patients had increased gray matter density (number of neurons) in neural networks that play a role in Parkinson’s disease. In a separate study, the same researchers found that an eight-week mindfulness program led to a significant improvement in motor symptoms.
Neurologists in Israel tested the effects of relaxation guided imagery on tremor in 20 Parkinson’s patients. Relaxation guided imagery dramatically decreased tremor in all patients, and in 15 of the 20 patients, tremor was completely eliminated for 1-13 minutes. Patients reported improvements lasting 2-14 hours afterward. In comparison, listening to relaxing music also reduced tremor but to a lesser degree, and self-relaxation had no significant effect on tremor.
In 2019, researchers in Hong Kong explored how mindfulness yoga compares with stretching and exercise training for people with Parkinson’s. Mindfulness yoga combines movements that improve balance and coordination with methods of stress release, relaxation, awareness, and focus. The study found that yoga had comparable benefits to stretching and resistance training in terms of motor symptoms and mobility, and that yoga had the added benefits of reducing psychological distress and improving spiritual well-being and health-related quality of life. Similarly, the Feldenkrais Method of somatic education improves quality of life scores and reduces depression in Parkinson’s patients.
In 2001, researchers demonstrated for the first time how a conscious experience is associated with the release of a neurotransmitter. During Yoga Nidra meditation, which reduces stress and is known as “yogic sleep,” participants experienced a 65% increase in endogenous dopamine release.
And in 2013, researchers used fMRI and EEG to observe brain activity of an experienced meditator as he entered jhana, a meditative state of ecstatic joy. They were able to see how he voluntarily stimulated his dopamine/opioid reward system using only his own internal mental processes. (If this sounds crazy to you, I promise it’s not. While I’ve been practicing mindful movement for many years, I am not an experienced meditator like the test subject, and I am able to do what is described in this study, albeit to a less intense degree. I find it very effective for reducing stress and boosting happiness. I think it can and should be pursued by beginning meditators and certainly by Parkinson’s patients.)
Comment les patients atteints de la maladie de Parkinson déclarent réduire ou éliminer leurs symptômes moteurs
The first story I heard of someone fully recovering from Parkinson’s disease was that of Howard Shifke. He describes how he recovered in his book Fighting Parkinson’s…and Winning—an inspiring book that I recommend to all.
Dans septembre 2009, alors qu'il travaillait sur son ordinateur, Howard Shifke a senti tout son corps trembler de l'intérieur. Howard avait vu sa mère souffrir de la maladie de Parkinson pendant 24 ans, et il est immédiatement entré dans un état de déni qu'il pourrait éventuellement avoir la même maladie. Mais il a commencé à se rendre compte que les symptômes apparaissaient progressivement depuis un certain temps : posture voûtée, équilibre qui se détériorait, démarche traînante, douleurs et raideurs musculaires et fatigue, entre autres.
Six semaines plus tard, il a consulté un neurologue et a reçu un diagnostic formel de la maladie de Parkinson. Howard est entré dans un autre état de déni - déni que son état était incurable. Il a choisi de ne prendre aucun médicament contre la maladie de Parkinson en raison des effets secondaires et a immédiatement créé un plan pour se remettre de la maladie de Parkinson sans médicament. Son approche comprenait la pratique quotidienne de la méditation, du Qigong médical et le passage à un régime végétarien.
Au fil des mois, Howard a découvert que son esprit critique, axé sur l'adrénaline et le jugement l'empêchait de progresser. Alors qu'il commençait à changer ses schémas de pensée habituels en ceux d'acceptation, de pardon, de compassion et d'amour, il a commencé à ressentir des améliorations notables de ses symptômes.
Le juin 9, 2010, neuf mois après qu'Howard a remarqué ses tremblements internes, ses symptômes ont soudainement diminué de 50 %. Trois jours plus tard, il s'est réveillé pour constater que ses symptômes avaient complètement disparu. Dix ans plus tard, il est toujours asymptomatique.
Howard now coaches people with Parkinson’s to help them reduce their symptoms and in some cases become symptom-free. You can read the stories of Tony C., Helen Gill, Marie, Pratima, and Betty M.—all of whom were diagnosed with Parkinson’s and used Howard’s Parkinson’s Recipe for Recovery® to become symptom-free. You can reach Howard through his website: https://www.fightingparkinsonsdrugfree.com
Quand j'ai lu pour la première fois comment les symptômes d'Howard avaient disparu assez soudainement, je me suis demandé quelle pouvait en être l'explication scientifique. Au fur et à mesure que j'en apprenais davantage sur la progression de la maladie de Parkinson et sur la façon dont les symptômes moteurs apparaissent à un seuil critique de production de dopamine/perte de neurones (estimé entre 30 % et 60 %), cela avait du sens. Lorsque les gens sont capables d'augmenter leurs niveaux de dopamine/nombre de neurones jusqu'à ce seuil critique, il est possible que les symptômes moteurs disparaissent aussi soudainement qu'ils ont commencé.
In 2016, doctors published a case report of a 78-year-old man’s remission of Parkinson’s symptoms, and cited meditation as a probable factor in his improvement:
« Nous présentons le cas d'un garçon de 78 ans qui, il y a 16 ans, a été diagnostiqué avec la maladie de Parkinson (MP) par un neurologue. Il a d'abord présenté un tremblement de la main gauche, une posture voûtée, une démarche traînante et des chutes fréquentes, qui ont finalement évolué vers des symptômes moteurs bilatéraux après 3 ans. Depuis 2012, ses symptômes et signes ont presque complètement disparu, et il a cessé toute pharmacothérapie pendant cette période. L'exactitude du diagnostic initial de MP est étayée par une présentation clinique appropriée, des antécédents de réponse positive à Sinemet et un scan SPECT DaT anormal ; ce cas suggère donc la possibilité d'une rémission des symptômes chez certains patients. Nous proposons que la longue histoire de pratique de la méditation du patient ait pu être un facteur contributif à cette amélioration, car il a été démontré que la méditation libère de la dopamine dans le striatum.
In his book The Brain’s Way of Healing, Norman Doidge describes how John Pepper consciously retrained his movements to overcome his foot drag and tremor. John was diagnosed with Parkinson’s more than 20 years ago, but first started getting symptoms almost 50 years ago. He decided to begin his recovery in 1998.
John s'est d'abord concentré sur sa marche, s'entraînant progressivement à supporter pleinement son poids et à utiliser les deux côtés de manière égale pendant qu'il marchait. Il lui a fallu un an pour intérioriser tous les changements et commencer à marcher normalement. Puis il a décidé de prendre le contrôle conscient de son tremblement. Maintenant, vous ne sauriez jamais en le regardant qu'il a la maladie de Parkinson. Il n'a pas une démarche traînante, il balance ses bras quand il marche et n'a aucun tremblement visible. Il ne semble pas rigide, est capable d'initier de nouveaux mouvements assez rapidement et a un bon sens de l'équilibre. John ne prend plus de médicaments contre la maladie de Parkinson depuis neuf ans.
In Pioneers of Recovery by Dr. Robert Rodgers, Bianca Mollé describes how she completely eliminated her motor symptoms using Qigong. When Bianca first began practicing Qigong, she immediately felt “one layer of pain strip away…there were many layers beneath that so it was a gradual process.” Soon she started forgetting to take her medication, because she wasn’t feeling tight and stiff. Her tremor was the last symptom to go away.
One year after Bianca began practicing Qigong, her neurologist declared her to be symptom-free. Two years later, the neurologist declared her to be Parkinson’s-free. Personally, she feels that she is still healing; she feels better and stronger every day. Bianca now offers online coaching for Parkinson’s patients and others with chronic illnesses, and you can watch her YouTube video about how she recovered.
Also in Pioneers of Recovery, Daniel Loney tells his story of how he has almost completely eliminated his motor symptoms using Tai Chi. When he was first diagnosed, he became very depressed, believing that there was no hope. His mother passed away shortly after his diagnosis, and he spent the next year mourning both her and his own life. Daniel’s condition went downhill rapidly; he almost quit practicing Tai Chi altogether, and he began to suffer from confusion, anxiety, and panic attacks.
Daniel a commencé à explorer des traitements alternatifs, notamment la médecine ayurvédique, le yoga, les massages, l'acupuncture et l'herboristerie chinoise. Il a estimé qu'ils ont tous aidé dans une certaine mesure. Finalement, il s'est rendu compte que dans sa pratique du Tai Chi, il avait tout ce dont il avait besoin pour se soigner.
Daniel left his stressful job and focused entirely on his recovery, putting an extreme emphasis on Tai Chi. His depression and mental symptoms went away almost immediately. As he regained strength, his tremor disappeared almost completely. He now feels very relaxed in his body; his stability, coordination, and strength have all improved; and he no longer stoops when he walks. It took about six months to a year for him to relieve his motor symptoms. Daniel now teaches Tai Chi for people with Parkinson’s in Israel. You can reach him through his website: https://www.taichiparkinsons.com
Parkinson’s patient Gord Summer has found vigorous exercise to be an essential part of his recovery. As he describes in Pioneers of Recovery:
« Vous commencez à vous épuiser. Ensuite, vous puisez dans votre ténacité… Je suis toujours richement récompensé après m'être poussé jusqu'à l'épuisement. Comment? Je marche le lendemain comme si j'étais un jeune garçon. Tout fonctionne mieux… Cela fait passer la rigidité au second plan. Il laisse facilement la maladie de Parkinson derrière lui pendant une journée entière. Cela a certainement été mon expérience personnelle.
Dans la maladie de Parkinson, les symptômes moteurs sont les signes externes et observables des changements qui se sont produits dans le cerveau. Lorsque les gens sont capables d'apporter des améliorations durables à leurs symptômes moteurs, c'est la preuve de réels changements qu'ils ont apportés à leur cerveau. Leurs histoires sont passionnantes et inspirantes et, espérons-le, révélatrices des changements futurs dans l'approche du traitement de la maladie de Parkinson.
Sheryl Marks Brown was diagnosed with a fast-progressing form of Parkinson’s in the summer of 2021. Tremors that normally take years to progress through the body took only five months to affect her entire body. Having cured herself in the 90’s from two autoimmune diseases, lupus and rheumatoid arthritis, Sheryl decided to try again to heal herself. She writes a blog to document the process, not knowing how it will end. You can read her blog and keep up with her inspiring journey of self-healing on her website, healingparkinsons.com.
In addition to mindfulness and mindful movement, there is a commonality among people who reduce or eliminate their motor symptoms: they believe they can get better. Expectation induces neurochemical changes in the brain. Researchers at the University of British Columbia demonstrated that simply believing their symptoms would improve triggered the release of dopamine in Parkinson’s patients. Further research replicated the results. Positron emission tomography (PET) scans show that belief stimulates the release of dopamine in the striatum of Parkinson’s patients, causing complete elimination of motor symptoms for a period of time. Dr. Joe Dispenza describes one such study in this video.
Likewise, studies like this, this, and this have shown that motor function in Parkinson’s patients improves when they receive placebo treatment or have the expectation that their symptoms will improve.
On the flip side, believing you will not improve deactivates the dopaminergic system. So in addition to stimulating neurogenesis and boosting dopamine with exercise and stress reduction, believing that you can improve is essential in your recovery.
Do you have Parkinson’s disease, and do you want to improve your motor symptoms? I recommend talking to Howard or Bianca, both of whom have eliminated their motor symptoms and now offer coaching. You may decide to follow their paths or create your own personalized prescription. And always remember: Your health is in your hands, and the more strongly you believe that you can improve and recover, the more likely it is that you will.
Lecture recommandée:
The Pain Relief Secret: How to Retrain Your Nervous System, Heal Your Body, and Overcome Chronic Pain by Sarah Warren, CSE
Somatics: Reawakening the Mind’s Control of Movement, Flexibility and Health by Thomas Hanna

