Nouvelle recherche sur la façon dont le stress affecte l'inflammation, la neurodégénérescence, le microbiome intestinal, le traitement du cancer et les relations
Le stress est une passion particulière pour moi. J'adore apprendre à réduire le stress négatif et je suis fasciné par la façon dont le stress affecte notre santé. Ceci est le premier d'une série d'articles que j'écrirai sur le stress dans les mois à venir.
Nous ne savons pas tout ce qu'il y a à savoir sur le stress. Dans l'ordre des choses, les scientifiques commencent seulement à comprendre la myriade de façons dont le stress chronique affecte us, et de nouvelles découvertes importantes sont faites chaque année. Dans cet article, je discuterai des recherches récentes sur ces sujets :
- Le stress endommage les mitochondries, entraînant des maladies et le vieillissement
- Le stress provoque une résistance aux récepteurs des glucocorticoïdes, ce qui augmente l'inflammation
- Le stress modifie les connexions neuronales, diminue le volume du cerveau et contribue à la maladie d'Alzheimer
- Le stress modifie la composition et le comportement des bactéries intestinales et provoque un « intestin qui fuit »
- Le stress augmente les métastases et diminue l'efficacité du traitement du cancer
- Le stress est contagieux au niveau cellulaire
Les mitochondries traduisent le stress psychologique en maladie et en vieillissement, fournissant une preuve biologique de la connexion corps-esprit
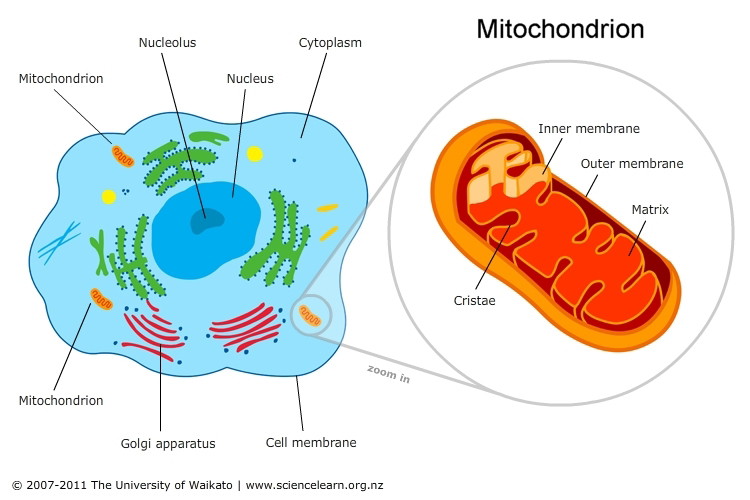
Les mitochondries sont des organites (sous-unités de cellules) présentes dans la plupart des cellules de notre corps. Les rôles les plus importants des mitochondries sont de produire de l'énergie pour les cellules, de réguler le métabolisme cellulaire et d'envoyer des signaux à d'autres cellules. Lorsque les mitochondries ne fonctionnent pas comme elles le devraient, des maladies graves impliquant de nombreux systèmes corporels différents peuvent en résulter.
A revealing 2018 review describes how acute and chronic stress affect mitochondrial structure and function, especially in the brain. These changes can then lead to inflammation throughout the body, increasing the risk of many inflammatory diseases. It’s believed that mitochondria play a role in regulating our physiological stress response, so stress-induced changes in mitochondria may result in even more stress. In addition, mitochondria have their own DNA, and damage to mitochondrial DNA caused by stress speeds up aging in mammals.
Evidence shows that mitochondria “sense, integrate, and signal information about their environment.” The growing body of evidence demonstrating how mitochondria translate stress into disease is exciting for the field of psychosomatic medicine, because it provides biological proof of how the mind and body interact.
Le stress chronique entraîne une résistance des récepteurs des glucocorticoïdes et une inflammation accrue
When we perceive stress, a series of hormones released in the brain triggers the adrenal gland to secrete hormones called glucocorticoids. These bind to glucocorticoid receptors, which are present in almost every cell in our body. Glucocorticoids play a critical role in regulating our stress response, including how much inflammation occurs.
Glucocorticoids must be able to bind to their receptors in order to do their job. Research now shows that chronic stress leads to glucocorticoid receptor resistance, making it difficult or impossible for glucocorticoids to bind. This resistance causes our inflammatory response to be longer and/or more intense, and our risk for suffering from the common cold, asthma, autoimmune diseases, cardiovascular disease, type 2 diabetes, and other inflammatory conditions is increased.
Le stress modifie les connexions neuronales, diminue le volume du cerveau et contribue à la maladie d'Alzheimer
Researchers from Zurich, Switzerland were surprised and excited by what they discovered about how stress changes the brain in a 2019 study published in Neuron.
When we perceive a threat, the neurotransmitter noradrenaline (aka norepinephrine) is released. Previous research has suggested that noradrenaline probably facilitates connections between parts of the brain. The research team from Zurich manipulated the brains of mice so that they could control when noradrenaline was released. They found that noradrenaline instantly “rewired” the mouse brains, making actual structural changes to neural connections. This finding suggests that the long-term effects of stress on the brain may be more profound than previously thought.
Dans l'étude, les changements structurels les plus importants se sont produits dans les zones du cerveau qui traitent les informations sensorielles (comme ce que nous voyons et entendons) et dans l'amygdale. L'amygdale est un groupe de noyaux du système limbique qui joue un rôle important dans les réponses émotionnelles de peur, d'anxiété et d'agressivité, ainsi que dans la mémoire et la prise de décision. L'amygdale est généralement hyperactive chez les personnes souffrant d'affections liées au stress, notamment l'anxiété et la dépression.
Chronic stress affects the amygdala by another means as well. Prolonged high levels of glucocorticoids stimulate neuron growth in the amygdala and make synapses more active and sensitive.
Stress and the release of glucocorticoids have also been shown to hardwire neural connections between the hippocampus and the amygdala, potentially creating a cycle in which the brain becomes stuck in a constant state of stress.
Of equal concern is the fact that effect that chronic stress has on decreasing brain volume and connectivity. Data from 2,231 participants in the Framingham Heart Study shows that people with increased levels of cortisol (one of the glucocorticoids) experience brain shrinkage and memory loss.
And a study of 103 healthy subjects showed decreased brain volume in the medial prefrontal cortex and the insula in people who had experienced repeated exposure to stress as well as those who had only experienced a recent stressful event. The affected areas of the brain regulate emotions, stress, reward regulation, memory, decision-making, and impulse control. The study authors suggest that this decrease in brain matter may help to explain the connection between stressful life events and an increased risk of depression, addiction, and other stress-related disorders.
Glucocorticoids have also been shown to decrease volume of the hippocampus, a part of the brain involved in memory, learning, attention, and ironically, regulating glucocorticoid secretion. So the more stress you experience and the more damage is done to your hippocampus, the less effective it is at regulating glucocorticoid levels, and the more glucocorticoids build up in your system. This is a vicious cycle that can make it difficult to reduce your level of stress.
There is a growing body of research on how stress contributes to Alzheimer’s disease. Based on current research, stress increases the expression of Amyloid Precursor Protein (APP) and the production of Aβ peptide, which then gets deposited into amyloid plaques. Amyloid plaques trigger an inflammatory response in the brain, and it’s believed that neurotoxic inflammatory substances contribute to the neurodegeneration that occurs in Alzheimer’s. Stress also elevates levels of the Tau protein, which leads to neurofibrillary tangle formation and neurodegeneration.
Le stress modifie la composition et le comportement des bactéries intestinales et provoque un « intestin qui fuit »
The human microbiome describes the trillions of microorganisms (aka microbiota or microbes) that reside within our body. Our gut microbiome has been getting a lot of attention lately because of the discoveries researchers have made about how our gut microbiome affects our overall health. These discoveries have led to a booming market for pre- and probiotics that claim to improve our gut health.
There is “bidirectional cross-talk” between our gut and our brain. Our enteric nervous system (aka ENS; the network of 200-600 million neurons in our digestive system) communicates with our central nervous system (CNS) in a number of ways, including via the vagus and pelvic nerves and systemically via immune system cells. The cross-communication between our digestive system and our brain means that there is a high rate of comorbidity of gastrointestinal and psychiatric disorders; for example, up to 94% of people with irritable bowel syndrome also suffer from a psychiatric disorder.
A 2019 study shows that social stress changes both the composition and the behavior of gut bacteria. After subjecting mice to repeated stress, the mice had significant differences in their gut bacteria, most notably in two types of bacteria linked to multiple sclerosis in humans. And in the stressed mice, some gut bacteria turned into destructive pathogens which are likely to infect tissue, trigger the immune response, and lead to autoimmune conditions.
A number of studies show how psychological stress increases gut permeability (aka “leaky gut”), a condition in which bacteria and toxins are able to leak through the intestinal wall, causing a wide variety of health problems.
We’re only beginning to understand the vast ways in which stress affects our gut microbiome, and vice versa. To learn more about this topic, check out The Mind-Gut Connection by Dr. Emeran Mayer.
Le stress augmente les métastases et diminue l'efficacité du traitement du cancer
A healthy immune system is our #1 line of defense against cancer. Unfortunately, a 2017 study showed that chronic stress suppresses the immune system’s response to cancer and reduces the efficacy of immunotherapy treatments. The researchers suggest that improving immune system function may improve the rate of success of conventional therapies like chemotherapy as well, because many of these therapies rely on the immune system for their efficacy. The researchers stated that “there is now pre-clinical evidence to suggest that treatments and lifestyle interventions to manage or reduce stress levels will improve the chances of these patients responding to therapies.”
A 2019 study made two important discoveries about how stress hormones affect breast cancer metastasis and treatment. First, the study showed that increased levels of stress hormones led to increased colonization (growth in secondary locations) and heterogeneity (diversity) of cancer cells—both of which make cancer more difficult to treat and decrease the survival rate of the patient.
Second, the study showed that synthetic derivatives of stress hormones (corticosteroids), which are often used as anti-inflammatories in cancer treatment, actually decrease the efficacy of chemotherapy. This finding suggests that corticosteroids should be used with caution in cancer therapy. One of the researchers, Mohamed Bentires-Alj, states that “These findings highlight the importance of stress management in patients…Moderate exercise and relaxation techniques have been shown to correlate with enhanced quality of life and greater survival in patients.”
Le stress est contagieux au niveau cellulaire
Si vous avez un membre de votre famille, un ami ou un partenaire amoureux qui est toujours stressé, vous avez peut-être remarqué l'effet que son stress a sur vous. Vous pouvez avoir l'impression que vous « absorbez » leur stress ou que vous ne pouvez pas vous détendre en leur présence. Eh bien, les scientifiques ont maintenant découvert à quel point le stress est contagieux au niveau cellulaire.
A 2018 study found that stress transmitted from someone else can change your brain in the same way that “real stress” (stress that you are exposed to) does. Corticotrophin-releasing hormone (CRH) neurons in the hypothalamus are activated when we perceive stress, and the researchers discovered that the activation of these CRH neurons in mice triggers the release of an “alarm pheromone” that chemically signals a non-stressed mouse nearby. Remarkably, this chemical signal activated CRH neurons in the non-stressed mice in the same way as in the mice that were exposed to stress.
Cette façon automatique de communiquer et de réagir au stress aide probablement diverses espèces à survivre en groupe; le membre qui détecte la menace peut alerter silencieusement les autres membres du groupe. Mais dans les relations humaines aujourd'hui, cela sert le plus souvent à augmenter le stress inutile que nous subissons.
And it turns out that you don’t even need to be physically close to someone in order to be affected by their stress. Researchers found that merely observing stressed people on video makes us release the stress hormone cortisol. This finding suggests that watching stressful television shows on a regular basis is likely not good for our stress level. On a larger scale, it speaks to the rising level of stress-related health conditions in the world, and suggests that we might experience stress in response to observing any stressed person in any manner, like on the street or via the internet. Stress is literally contagious, and we are all more connected than ever before.
Even our pets are affected by our stress level. A 2019 study found that owners with high levels of cortisol have dogs with high levels of cortisol, and owners with low levels of cortisol have dogs with low levels. Based on the study’s assessment of the owners’ and dogs’ personalities, the researchers determined that dogs mirror their owner’s stress, and not the other way around.
En conclusion
Bien que nous ne sachions pas tout ce qu'il y a à savoir sur les effets négatifs du stress psychologique chronique, ce que nous savons est suffisant pour mettre la réduction du stress au premier plan avec l'exercice et une alimentation saine en matière de santé et de longévité. Prendre le temps de se détendre peut sembler égoïste, indulgent et inutile, mais plus vous lirez de recherches sur ce sujet, plus vous vous sentirez obligé d'intégrer la relaxation et les soins personnels dans votre routine quotidienne. Réduire votre niveau de stress et modifier vos réactions automatiques au stress améliorera également immédiatement vos relations - essayez-le et voyez !
Lecture recommandée:
The Pain Relief Secret: How to Retrain Your Nervous System, Heal Your Body, and Overcome Chronic Pain by Sarah Warren, CSE
Somatics: Reawakening the Mind’s Control of Movement, Flexibility and Health by Thomas Hanna