Comment se remettre du syndrome de fatigue chronique ?
Dans mon précédent article sur le syndrome de fatigue chronique (2020 ), j'ai abordé les symptômes de la maladie, les causes possibles et les recherches sur les tests, le diagnostic et le traitement. Dans cet article, j'aborde quelques-uns des moyens par lesquels les personnes atteintes du syndrome de fatigue chronique peuvent inverser leur état de manière naturelle.
L'encéphalomyélite myalgique/syndrome de fatigue chronique (EM/SFC) survient généralement parce que les systèmes de l'organisme, en particulier le système immunitaire, sont débordés par divers facteurs de stress : infections, toxines environnementales, aliments inflammatoires, carences en nutriments et stress.
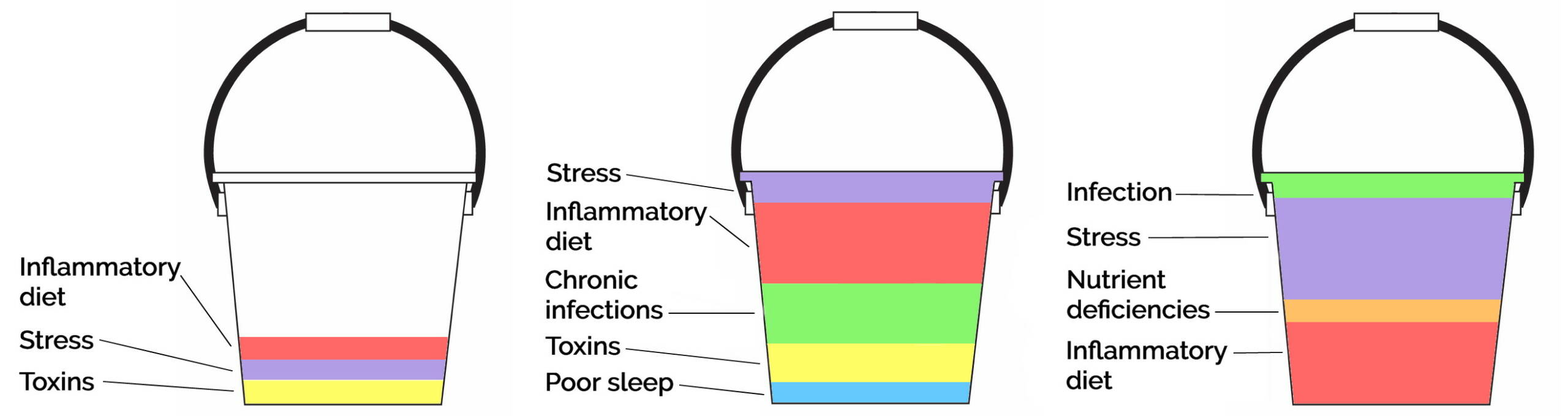
This is often referred to as “total body burden.” Everyone with any type of chronic disease needs to consider their total body burden. As Palmer Kippola describes in Beat Autoimmune, it helps to imagine that we each have a bucket that fills up throughout the course of our lifetimes. Each of us has a different combination and number of stressors in our bucket.
Bien qu'il puisse parfois sembler qu'une chose spécifique ait déclenché une maladie, nous devons également tenir compte de ce qui remplit notre réservoir. Par exemple, dans le deuxième casier ci-dessous, l'organisme de la personne est tellement accablé par une alimentation inflammatoire, des infections chroniques, des toxines et un manque de sommeil qu'un seul événement stressant peut déclencher une maladie. Dans le troisième cas, l'organisme de la personne est tellement surchargé par le stress, une alimentation inflammatoire et des carences en nutriments qu'une seule infection est susceptible de déclencher une maladie chronique. En revanche, le premier seau montre une personne dont la charge corporelle totale est très légère ; cette personne se remettra rapidement d'une infection, d'une exposition à un produit toxique ou d'un épisode de stress.
La bonne nouvelle, c'est que nous pouvons progressivement vider notre seau en éliminant les infections chroniques, en réduisant notre exposition aux substances toxiques et en nous désintoxiquant, en améliorant la santé de notre microbiome intestinal, en remédiant aux carences en nutriments, en réduisant le stress et en augmentant l'activité physique de manière appropriée. Toutes ces mesures servent à renforcer notre système immunitaire et à améliorer la capacité de notre organisme à faire face aux facteurs de stress auxquels nous sommes exposés chaque jour.
If you are just beginning this journey, I recommend seeking out a qualified functional medicine practitioner who can order the appropriate lab tests and guide you through the process of healing.
Je vous recommande également de lire un ou plusieurs de ces ouvrages, qui offrent des conseils détaillés sur la manière de réduire la charge corporelle totale et de guérir d'une maladie auto-immune :
Beat Autoimmune by Palmer Kippola
The Autoimmune Solution by Dr. Amy Myers
The Wahls Protocol by Dr. Terry Wahls
Brave New Medicine by Dr. Cynthia Li
Éliminez les infections chroniques
Approximately 70% of ME/CFS cases are preceded by a viral infection. Some viruses that frequently lead to the condition are Epstein-Barr virus (EBV), cytomegalovirus (CMV), varicella-zoster virus (VZV), human herpesvirus (HHV-6, HHV-7, HHV-8), human parvovirus B19 (B19V), and enteroviruses. There have been dozens of reported outbreaks of ME/CFS, most of which followed viral outbreaks, and some of which occurred due to toxin exposure. Bacterial, fungal, or parasitic infections may also trigger the condition.
Il est important de savoir que les virus peuvent rester latents dans l'organisme pendant des années, voire des décennies. Elles peuvent ne pas provoquer de symptômes visibles jusqu'à un certain moment de la vie, lorsque votre système immunitaire est compromis - en d'autres termes, lorsque votre seau se remplit et déborde. Vous pouvez également souffrir d'une infection bactérienne, fongique ou parasitaire sans le savoir.
About half of patients with post-COVID syndrome also fulfill the criteria for ME/CFS. And COVID infection often reactivates latent viruses in both ME/CFS patients and healthy controls. ME/CFS patients exhibit stronger antibody responses after COVID infection, especially to Epstein-Barr Virus (EBV). These patients also had elevated antibodies to EBV prior to COVID infection, which is evidence of ME/CFS patients having a higher viral load than healthy controls.
Unfortunately, studies of antiviral drugs for ME/CFS have shown limited success in treating patients. This may be because the patients are compromised by so many types of stressors—infections, toxins, diet, nutrient deficiencies, stress, etc.—that addressing just one source of stress on the immune system is not enough.
You can talk to your doctor or functional medicine practitioner to get tested for a variety of chronic viral, bacterial, parasitic, and fungal infections. In Beat Autoimmune, Palmer Kippola offers an excellent step-by-step guide on how to assess whether or not you might have a chronic infection, how to get tested, and how to go about clearing infections naturally. Her strategies include increasing cellular energy, strengthening the immune system, taking herbal antimicrobials, and more.
Réduire l'exposition aux substances toxiques et se désintoxiquer
It’s easy to dismiss the idea of synthetic chemicals affecting our health, especially if we don’t have any noticeable chemical sensitivities and aren’t aware of any specific incidents of exposure. But synthetic chemicals are all around us: in the air we breathe, the water we drink and bathe in, the food we eat, the clothes we wear, and the furniture we sit on. A hundred years ago, there were virtually no synthetic chemicals used in commerce, yet today there are nearly 80,000 different chemicals in products we use every day (some sources estimate more). Frighteningly, less than 5% of these chemicals are tested for safety in humans before being used in commercial products.
Synthetic chemicals and other toxins found in the environment (such as heavy metals and mold) can trigger symptoms similar to ME/CFS, can increase risk of the disease by overloading the body’s detoxification system, and can damage mitochondria, which produce energy for our cells.
These synthetic chemicals make their way into our bodies—through our lungs, skin, and digestive system—and lodge themselves in the cells of our body. The average adult has around 700 contaminants in their body, while newborns are born with about 200 chemicals in their umbilical cord blood.
“Chemicals get into our body, bind to our tissue, and change the very structure of our body parts, whether it be our thyroid, adrenal gland, or myelin sheath, etc., into a structure that our immune system doesn’t recognize. This new structure becomes a neoantigen—a new foreign substance or enemy bound to human tissue for the immune system to attack. Just doing its job, the immune system then produces “autoantibodies” to attack the new antigen—that is, our own new, foreign-looking tissue.” -Dr. Aristo Vojdani, Beat Autoimmune, p. 153
De nombreux produits chimiques toxiques sont stockés dans nos cellules graisseuses. Notre corps fait cela pour éloigner les toxines de notre circulation sanguine et de nos organes. En fait, de nombreux produits chimiques sont appelés obésogènes parce qu'ils créent des cellules adipeuses et sont souvent stockés dans l'abdomen sous forme de graisse ventrale. Pour que ces toxines soient éliminées de l'organisme, elles doivent être transformées de substances liposolubles en substances hydrosolubles. Cela leur permet d'être excrétés par l'air que nous expirons, par notre sueur et par notre urine et nos excréments.
Lorsque les toxines sont libérées des cellules graisseuses, elles sont transformées en métabolites réactifs. À ce stade, ils deviennent plus dangereux car ils circulent dans le corps. Il est donc essentiel qu'ils soient excrétés le plus efficacement possible. Une autre structure chimique doit s'attacher à la toxine pour la rendre soluble dans l'eau et l'"escorter" hors de l'organisme. La meilleure façon d'y parvenir est d'adopter une alimentation riche en nutriments capables de se lier aux toxines. Les experts recommandent en particulier les aliments suivants :
- Légumes crucifères (chou frisé, brocoli, chou-fleur, chou)
- Feuilles vertes foncées
- Légumes et fruits de couleur vive
- Aliments contenant du soufre (ail, oignons, œufs)
- Aliments riches en acides aminés (bouillon d'os, viande, volaille, poisson, épinards)
- Viandes d'organes
- Iode (à partir d'algues ou en complément)
- Minéraux (provenant du sel de mer non raffiné)
Vous pouvez également envisager de vous supplémenter avec une variété de "liants", des substances naturelles qui se lient aux toxines et leur permettent d'être excrétées. Il s'agit notamment de la chlorelle, de la coriandre, du charbon actif et de l'argile de qualité alimentaire.
The good news is, we can reduce our toxic load quite a bit on our own. Experts estimate that we can reduce well over half of our toxic load simply by removing chemicals from our homes, drinking filtered water, and cleaning up our diets. Dr. Joseph Pizzorno estimates that 70% of our toxic load comes from the food we eat, so switching to organic, unprocessed food is the most important change we should make if we want to detoxify our bodies.
Si vous souhaitez tester la présence de produits chimiques synthétiques et d'autres toxines telles que les métaux lourds, les moisissures et les endotoxines, votre professionnel de la santé peut vous prescrire divers tests de laboratoire. Lorsque vous recherchez des substances chimiques, il est important d'effectuer un dépistage de l'immunoréactivité chimique, qui indique les substances chimiques spécifiques auxquelles votre système immunitaire réagit (plutôt que toutes les substances chimiques présentes dans votre corps).
Both Palmer Kippola and Dr. Terry Wahls offer detailed advice on:
- Comment se faire dépister pour diverses toxines ?
- Comment réduire la charge toxique de notre alimentation
- Comment remplacer les produits que nous utilisons à la maison par des produits exempts de toxines ?
- Comment rendre notre environnement domestique moins toxique
- Comment optimiser le système naturel de désintoxication de notre corps ?
- Comment prendre certains suppléments pour augmenter la désintoxication
- Comment utiliser des stratégies de désintoxication plus "lourdes" comme les intraveineuses nutritionnelles et la thérapie par chélation ?
Another book I enjoyed is Sweat: Uncovering Your Body’s Hidden Superpower by Justin Glaser. He discusses the Niacin Sauna Protocol, which helped roughly 5,000 first responders and emergency workers who were present at Ground Zero after the 9/11 attacks and were exposed to a wide range of toxic substances through the air. These workers, who experienced a wide range of health problems, worked with the Foundation for Advancements in Science and Education to create a detoxification protocol. The sauna protocol allowed the majority of the workers to eliminate their pulmonary medication. They regained their health and vitality, had improved thyroid function, lost weight, returned to work, and reported a “total, utter transformation.”
Améliorez la santé de votre microbiome intestinal
The gut microbiome, also called the gut microbiota or gut flora, is the collection of bacteria, fungi, and viruses that live in our digestive tract. Our gut microbiome protects us from pathogens that enter through our gut, maintains our gut lining, and metabolizes food. It also affects our systemic immunity, and even our behavior and cognition through the gut-brain axis. About 70% of our immune system is in our gut, so when trying to heal from any chronic illness, improving gut health is essential.
Researchers have measured biomarkers related to intestinal barrier dysfunction and bacterial dislocation (movement of bacteria through the gut lining and into the rest of the body, where it causes health problems) in ME/CFS patients. They’ve found that intestinal permeability (leaky gut) and related inflammation are associated with symptoms of autonomic dysfunction in chronic fatigue syndrome.
The gut dybiosis present in ME/CFS may be caused by a number of factors, including antibiotic use, inflammatory foods, environmental toxins, chronic infections, pharmaceuticals, and stress.
Scientists are exploring ways to manipulate and improve the health of the gut microbiome in ME/CFS patients. One option is taking probiotics, which add live, beneficial microorganisms to the gut. Probiotics can be consumed in supplement form, and are also found in fermented foods like yogurt, sauerkraut, kimchi, and apple cider vinegar. In order for the probiotics to survive, you need to feed them with prebiotics, which are fermentable soluble fiber. Foods high in this type of fiber are plant foods, including potatoes, certain grains and legumes, asparagus, garlic, onion, and many common fruits.
Eliminating inflammatory foods is another essential step in improving the health of the gut microbiome. While we each have certain foods that are particularly inflammatory for us, processed foods are inflammatory for everyone. They contain many unnatural substances, like added sugar, trans fat, and chemicals like food additives and preservatives, as well as high levels of omega-6 fatty acids. So, switching to a diet of whole, unprocessed foods is important for anyone with a chronic inflammatory disease.
It’s also advisable to go on an elimination diet for at least 30 days so that you can identify any specific food intolerances, which are linked to ME/CFS. The Whole30 diet is a great place to start. You may find that dairy products are contributing to your inflammation; many people are unable to digest lactose, and casein causes autoimmune reactions in many people as well. You may also find that gluten, a type of lectin, is contributing to your symptoms. To learn more about how your diet could be contributing to your inflammation, please read How Diet Affects Inflammation and Chronic Pain. The three autoimmune books I linked to at the beginning of the article also give detailed recommendations on dietary changes to make when healing from an autoimmune condition.
The ultimate type of elimination diet is, of course, fasting. Therapeutic fasting immediately eliminates all foods that may be triggering inflammation. Fasting induces the state of autophagy, by which the body gets rid of old, damaged cells and replaces them with new, healthy cells; this is especially important when trying to heal a damaged gut lining. Autophagy also regenerates the immune system and clears bacteria and viruses from the body, potentially clearing chronic infections. Intermittent fasting is recommended as a way to strengthen the immune system to prevent against infections like COVID, and extended fasting has been found to reduce symptoms of long-term COVID. If you decide to try fasting, you should do so under the supervision of your health professional, and start slowly with intermittent water-only fasting.
A treatment called fecal microbial transplantation (FMT) is also being researched for ME/CFS patients. Fecal transplantation, also called bacteriotherapy, is the transfer of stool from a healthy donor into the GI tract of another person. The procedure has been used in Chinese medicine for at least 1,700 years and is becoming increasingly mainstream. A 2012 study of FMT found that the treatment led to a 70% success rate and 58% sustained positive response in ME/CFS patients. A 2019 study compared FMT to standard nutritional treatments, like pre- and probiotics and dietary advice. The researchers found that the ME/CFS patients who received FMT experienced greater improvements than the standard treatment group.
Remédier aux carences nutritionnelles
Des carences en certaines vitamines et minéraux peuvent affaiblir le système immunitaire. Micronutrients agissent comme des antioxydants pour protéger les cellules saines des radicaux libres, soutiennent la croissance et l'activité des cellules du système immunitaire et contribuent à la production d'anticorps. La recherche montre que les personnes présentant des carences nutritionnelles sont plus susceptibles de contracter des infections et des maladies chroniques.
Certain nutrient deficiencies are associated with severity and exacerbation of ME/CFS symptoms. These include vitamin C, vitamin B complex, sodium, magnesium, zinc, folic acid, l-carnitine, l-tryptophan, essential fatty acids, and coenzyme Q10.
While it is always preferable to get these nutrients from whole, unprocessed foods, sometimes eating the ideal diet isn’t enough. It may be necessary to take supplements for a period of time in order to get nutrients up to healthy levels. It also can be helpful to take supplements due to the lack of nutrients in our food supply; the soil we grow our food in is depleted of nutrients. Modern farming techniques prevent the soil’s ability to naturally restore minerals. The use of phosphate-based fertilizers decreases the levels of nutrients even further. It’s estimated that the mineral content of vegetables has declined by as much as 80-90% over the past century.
A 2014 study of 38 ME/CFS patients found that taking a multivitamin, multi-mineral supplement for two months led to significant improvements in fatigue, autonomic nervous system function, headaches, sleep quality, and antioxidant levels. Another study of 67 subjects with chronic fatigue found that just one week of supplementation with a membrane glycophospholipid-antioxidant-vitamin mixture resulted in a reduction in fatigue of 36.8%.
Studies of individual nutrients, like CoQ10, vitamin B-12, D-ribose, and essential fatty acids, have also found significant benefits for improving ME/CFS symptoms, including energy, sleep, mental clarity, pain intensity, and general well-being.
Avant de commencer à prendre des suppléments de vitamines ou de minéraux, vous devriez consulter votre médecin pour vous assurer qu'ils n'interagissent pas avec les médicaments que vous prenez. Afin d'adapter votre supplémentation à vos besoins, vous pouvez envisager de faire une analyse sanguine complète des vitamines et des minéraux. Votre professionnel de santé peut vous prescrire ce type de test, ou vous pouvez les commander en ligne auprès de laboratoires d'analyses à domicile.
S'exposer régulièrement et modérément au soleil
There are many benefits of regular sun exposure for chronic fatigue patients: producing adequate vitamin D, strengthening the immune system, and producing adequate serotonin and melatonin. Due to over-avoidance of the sun, the western world is suffering from widespread vitamin D deficiency. Researchers state that this public health issue has grown to the level of a pandemic.
Malheureusement, la population générale souffre davantage de problèmes de santé dus à un manque d'exposition au soleil qu'à un excès de soleil. La carence en vitamine D est associée à un large éventail de problèmes de santé, notamment le cancer, les maladies auto-immunes, l'hypertension, les maladies infectieuses, le rachitisme, l'ostéopénie, l'ostéoporose et les fractures osseuses.
L'exposition aux rayons UV du soleil est le moyen le plus efficace pour l'homme d'obtenir suffisamment de vitamine D pour rester en bonne santé. Peu d'aliments contiennent de la vitamine D, et les aliments enrichis en vitamine D ne couvrent généralement pas nos besoins quotidiens.
Research has found that ME/CFS patients have moderately to severely suboptimal vitamin D levels. Scientists recommend that chronic fatigue syndrome patients obtain regular adequate sun exposure and eat foods high in vitamin D. Patients whose levels do not rise to optimal levels with these practices should consider vitamin D supplementation.
Vitamin D deficiency also increases susceptibility to chronic infections such as COVID. Research shows that maintaining adequate vitamin D levels helps to keep the immune system strong and prevent the “cytokine storm” (excessive inflammatory reaction) that can occur during COVID, the flu, and other viral infections such as the Epstein-Barr virus.
Research shows that regular sun exposure can have more benefits for the immune system than simply increasing vitamin D production. Scientists at Georgetown University Medical Center found that sun exposure mobilizes infection-fighting T-cells. Sun exposure can protect against autoimmune conditions, as well as many common types of cancer including breast, ovarian, colon, pancreatic, prostate, and Hodgkin lymphoma. Researchers suggest that sun exposure can modulate levels of immune cells, increasing anti-inflammatory cytokines and decreasing pro-inflammatory cytokines.
Serotonin is a neurotransmitter that helps to regulate mood, social behavior, learning, cognition, memory, cardiovascular function, sensorimotor function, pain sensation, appetite, bowel motility, bladder control, sleep, and sexual desire. Serotonin is typically low in people with chronic fatigue syndrome. The more bright light that our skin and eyes are exposed to, the more serotonin we produce.
Serotonin is also a precursor to melatonin, a hormone best known for regulating our sleep-wake cycle. It also functions as an antioxidant and anti-inflammatory, protecting against infection, inflammation, and autoimmunity, and also regulates blood pressure and reproductive function. Melatonin supplements have been found to be effective for reducing fatigue and improving the quality of life in ME/CFS patients. But since melatonin supplements vary in quality, and since the nervous system can become adapted to supplements, it is far preferable to maintain melatonin levels by getting regular sun exposure. You can read this article to learn more about serotonin and melatonin.
You can reference this chart as a general guide for how much sun exposure is ideal for your skin type based on the UV index. Many weather apps on smartphones show the current UV index of your location. When UV index is lower, longer sun exposure is necessary. It’s important to expose as much of your skin as possible, as each area of skin can produce a fixed amount vitamin D at a time. The darkest-skinned people need up to ten times more sun exposure than the fairest-skinned people, since darker skin absorbs fewer UV rays. To learn more about how moderate sun exposure improves health, I recommend reading The Healing Power of the Sun by Dr. Richard Hobday.
Réduire le stress
Stress typically plays a role in the development and exacerbation of chronic fatigue syndrome. Many ME/CFS patients report emotional or physical stress as a trigger for the onset of their disease. Recall the bucket image from the beginning of the article: If your bucket is already almost full, an episode of acute stress can easily overwhelm your immune system. Chronic stress can gradually fill up your bucket, putting your immune system in a state where any challenge could trigger disease.
Humans have evolved to deal with acute stressors quite well, but most of us today experience chronic stress that never goes away. This type of stress keeps levels of pro-inflammatory cytokines high, keeping the immune system stuck in a dysregulated, inflammatory state all the time and increasing risk of chronic disease. Chronic stress also increases the risk of activating latent viruses, which are known to be a contributor to ME/CFS.
Stress also causes gut dysbiosis, which is an issue for most, if not all, chronic fatigue patients. Stress contributes to intestinal permeability, and allows bad gut bacteria to flourish and good bacteria to die off. As I discussed earlier, the gut microbiome and gut lining make up about 70% of the immune system, so improving the health of the gut is essential when trying to heal from any autoimmune condition. Reducing stress is one important way to improve gut health.
Scientists use the term “allostatic load” to describe the cumulative burden of chronic stress on the body. It can be measured by testing biomarkers of the immune, cardiovascular, neuroendocrine, and metabolic systems. When combined and assessed, the levels of these biomarkers provide a general picture of physiological dysregulation. Measuring allostatic load gives health professionals a way to quantify the risk of poor health and chronic disease. Some scientists recommend assessing allostatic load by using an integrated approach that combines biomarkers with an interview and/or a self-rated questionnaire (the PsychoSocial Index). This approach allows self-reported psychological distress, life events, behavior, and general well-being to be taken into account.
Allostatic overload is associated with poorer health outcomes, such as increased rate of death and increased risk of cancer. A study of ME/CFS patients found that they were 1.9 times as likely to have a high allostatic load index than healthy control subjects. The three biomarkers that were most strongly associated with chronic fatigue syndrome were waist:hip ratio, aldosterone and urinary cortisol.
Palmer Kippola includes an excellent chapter on stress in her book Beat Autoimmune. She discusses how stress leads to disease, and the roles of childhood stress, stress perception, and personality types. She includes a stress self-assessment, and goes into detail about many helpful ways to reduce stress, improve coping, increase positive emotions, and retrain the nervous system.
Augmenter l'activité physique
L'activité physique, quelle qu'elle soit, peut sembler incroyablement difficile, voire impossible, lorsque vous souffrez du syndrome de fatigue chronique. Cependant, il a été démontré que l'exercice réduit les symptômes de l'EM/SFC et diminue l'inflammation. La meilleure façon d'aborder l'exercice est de commencer par de courtes séances de mouvements faciles, en maintenant votre fréquence cardiaque basse, et en augmentant progressivement la durée et l'intensité des séances en fonction de vos capacités.
A 2017 review of eight studies, which included 1518 ME/CFS patients, found that the patients had less fatigue and improved sense of well-being following exercise therapy. The symptoms that improved most as a result of exercise were sleep, physical function, and self-perceived general health.
Moderate-intensity exercise reduces levels of pro-inflammatory cytokines while increasing production of anti-inflammatory cytokines; in other words, exercise reduces inflammation. Researchers report that exercise strengthens the immune system and triggers a defense mechanism against infections.
Depending on the duration and intensity of exercise, the number of anti-inflammatory immune cells can increase by 50% to 400%. However, the levels of these immune cells falls to pre-exercise levels within three hours, so regular exercise is essential to improving the strength of the immune system and protecting against disease.
Exercise doesn’t have to be complicated or expensive—simply taking regular walks has measurable and significant effects on the immune system. Studies show that when sedentary people start walking for 45 minutes five days per week, they have a significantly reduced risk of upper respiratory tract infections, and this reduced risk continues to become greater over time with continued regular walking. Shorter exercise sessions have benefits too. Walking for just 20 minutes per day five days per week led to 43% reduction in upper respiratory tract infections in just 12 weeks.
If you have ME/CFS and want to start exercising, it’s important to start slowly and pace yourself. You can apply the concept of pacing to the activities of your daily life as well. When it comes to exercise, you may need to limit yourself to very short sessions to start with. For example, take a five-minute walk outside, and notice how you feel afterward and the next day. Very gradually increase the length of time that you walk, only as you are able to while feeling good afterward. Increased fatigue is a sign that you’ve done too much.
If walking and other types of exercise are too tiring or painful, Clinical Somatics can be a wonderful way to start moving your body gently. The movements calm the nervous system and reduce stress, and ME/CFS patients have reported finding the exercises very helpful in their recovery. Clinical Somatics exercises can be practiced on the floor or in a chair, and can be modified to suit your needs.
Aller de l'avant dans votre processus de guérison
En lisant cet article, vous avez peut-être eu des idées ou des intuitions sur la façon dont vous voulez avancer dans votre processus de guérison. Il est utile de noter ces idées et d'en dresser la liste afin de ne pas avoir à les garder toutes en tête ! Au lieu d'essayer de traiter tous vos facteurs de stress en même temps, choisissez-en un ou deux à explorer cette semaine. Envisagez de prendre rendez-vous avec un praticien qualifié et expérimenté en médecine fonctionnelle. Passez 15 minutes au soleil chaque jour. Commencez par éliminer les aliments transformés et privilégiez les aliments entiers et non transformés. Il suffit d'avancer pas à pas et vous serez dans la bonne direction.
Lecture recommandée:
The Pain Relief Secret: How to Retrain Your Nervous System, Heal Your Body, and Overcome Chronic Pain by Sarah Warren, CSE
Somatics: Reawakening the Mind’s Control of Movement, Flexibility and Health by Thomas Hanna

